The Biden-Harris Administration identified improved indoor air quality as an essential tool to fight the spread of airborne diseases in the American Pandemic Preparedness Plan last September – and the National COVID-19 Preparedness Plan prioritized it again earlier this month.
As part of the efforts, on March 29th, 2022, clean air experts gathered at an online event hosted by the White House’s Office of Science and Technology Policy (OSTP) to discuss the most effective ways to ensure clean air and manage air pollutants.
The panel consisted of the following experts:
- Alondra Nelson (leads the White House Office of Science and Technology Policy)
- Dr. Zeynep Tufekci (Associate Professor at The University of North Carolina at Chapel Hill and writer at The New York Times).
- Dr. Joseph Allen (Associate Professor at Harvard T.H. Chan School of Public Health).
- Dr. Linsey Marr* (Professor of Civil and Environmental Engineering, Virginia Tech).
- Kenneth Martinez** (Chief Science Officer, Integrated Bioscience and Built Environment Consortium).
- Tracy Enger (Team Leader/Program Analyst, Indoor Environments Division, United States Environmental Protection Agency).
*Dr. Linsey Marr was also part of the C.L.E.A.N. Lessons Learned session, “Communities Of Faith: Safely Gathering In COVID-19 Times.” Watch it here.
** Kenneth Martinez was also part of IBEC’s online webinar “Protecting Our Most Vulnerable Workers: Challenges, Solutions & Invisible Barriers.” Watch it here.
Otherwise, keep reading to get a summary of the key aspects discussed on March 29th, 2022. You will be able to learn how to improve the air quality while gathering indoors.
Is clean indoor air necessary? Why?
Alondra Nelson

There’s a need to have cleaner indoor air, and this need is not new. Luckily, there are multiple ways to manage indoor air pollution, such as improving ventilation indoors, strengthening air filtration, and disinfecting the air. It’s an investment that will benefit future generations and improve people’s long-term health.
It has been demonstrated that five air changes per hour can reduce transmission risk by 50% or more. This is an achievable goal for our schools and our workplaces. Improving indoor air quality does not conflict with our energy efficiency goals. It is not a dichotomy, and we can work on both clean and energy-efficient air simultaneously.
The truth is that clean air is about more than just COVID-19. It helps improve public health and fight against other common airborne diseases like influenza and indoor pollution sources like smoke and gas stoves that can impact our respiratory health.
This is why the Elementary and Secondary School Emergency Relief Fund made available $122 billion to help schools prevent the spread of COVID 19, including performing ventilation improvements. Your school districts will know how to apply for these funds through your state education agency.
Following the same effort, $350 billion were provided through the state and local fiscal recovery funds to help state, local and tribal governments support their local businesses, nonprofits, and the public sector. You can reach out to your local government to learn more about these resources.
The importance of our history and clean indoor air
Dr. Zeynep Tufekci

Historically, we’ve always struggled to figure out how diseases spread. We didn’t have the germ theory of disease until the 19th century. Prior, there was a belief that foul air, which was smelly, was the cause of many diseases, forming the miasma theories of disease. We were onto something because poorly ventilated and smelly places are usually polluted places that are more likely to be inhabited by disadvantaged populations.
The miasma theory caused challenges in understanding waterborne diseases because it wasn’t the smelly water that made people sick. It was clear water that was perfectly fine to the eye and other senses. In the 20th century, a theory developed. The idea was that what spreads diseases are those particles we emit from our mouths; they are called droplets or watery stuff that falls to the ground.
Then, a second theory developed, inciting that the aerosols we breathe are also a significant way of disease transmission. These are also more concentrated around the person, which makes distance matter. As well, they don’t necessarily fall to the ground.
For the rest of the 20th century, scientists accumulated evidence about aerosol transmission but experienced sociological hurdles and were left without assistance or funding.
Fast forward to the pandemic, the droplet dogma immediately got repeated as it was happening. However, emerging evidence showed the virus was traveling long distances, it wasn’t transmitting outdoors, and scientists wondered why. Organizations realized something was wrong with the previous logic, and sadly, the evidence wasn’t recognized soon enough.
By acknowledging the airborne/aerosol nature of viruses such as COVID-19 and influenza, we get an incredible toolkit that allows us to control many venues and is essential for equity. This is an incredible opportunity to do with indoor air what we did to sanitation and water.
Let’s talk about the built environment
Dr. Joseph Allen

Our buildings can make us sick or keep us well. If you acknowledge that airborne spread is happening, then the building matters.
Early in the pandemic, the airborne spread was missed because we focused on surfaces. Suppose you increase ventilation filtration and reduce the amount of virus in the air. In that case, you reduce the intensity of exposure or the inhaled dose, the amount of virus you inhale, which decreases your risk.
We’ve designed our buildings to bare minimum standards, not health-based standards. We have a minimum design standard for our buildings. But then, over time, we don’t give them a tune-up, and the building starts to perform worse.
If you want to make your building safe from COVID-19 and other viruses, first and foremost, bring that building back up to the way it was designed. When you understand your systems, you can start to make these improvements to go above and beyond.
Many studies have shown higher ventilation rates, higher filtration associated with better reading scores, better math scores for students, and decreases in school absenteeism.
The benefits don’t just stop with schools; we see this in offices and workers everywhere. Higher ventilation rates are associated with fewer missed workdays, better cognitive functions, thinking more clearly, less fatigue, and fewer headaches.
Dr. Joseph Allen’s research on the benefits of ventilation and cognitive function shows that at the cost of $40 per person per year, we see benefits to the business on the order of six to $7,000 per person per year.
The Massachusetts Institute of Technology (M.I.T.) did a study showing that buildings that are designed and operate to a healthy building standard command effective rents four to 8% higher per square foot. So healthy buildings are just good business decisions.
We’re an indoor species; we spend 90% of our time indoors. It’s intuitive and logical then that the indoor environment has an outsized impact on our health, and we’ve been ignoring it for too long.
How does COVID-19 Spread?
Dr. Linsey Marr

The Coronavirus is in our respiratory fluid, it’s in saliva, snot, and the fluid lining our lungs, and it comes out not as a naked virus but in tiny bits of this fluid.
Medical experts had thought or assumed that transmission was occurring by large droplets that come out of our mouths when we cough or sneeze, and they contain viruses. These droplets could spray into someone’s eyes, nostrils or lips or potentially contaminate another object. These droplets are pretty large, and they typically fall quickly to the ground within six feet.
However, this is not precisely what happens. We do release some large droplets when we talk, cough or sneeze. But we also release hundreds of tiny ones that are too small to see, called aerosol particles or just aerosols.
These aerosols can carry the virus. They carry more virus than we would expect, given their small size. And they’re small enough that they can float around in the air for a long time. These aerosol particles can build up in the space, especially if the infected person is still there.
Aerosols float around just like cigarette smoke, they don’t stop at six feet, and they can travel quickly. Even if the air in the feels still, there’s always some movement carrying these tiny particles around. If the indoor setting is poorly ventilated, those will continue to build up over time.
We need to reduce the number of aerosol particles, and we have well-established ways of doing that. The first is ventilation. Move more air through, bringing in virus-free outdoor air and pushing out the stale air that contains all the viral aerosols. This will reduce or dilute the amount of virus in the.
This can be as simple as opening the windows or adjusting the heating, ventilation, and air conditioning system to bring in more outdoor air and use less recirculated air.
Filtration is another good option for reducing the number of aerosols. We can rely on a very efficient HEPA filter for trapping viruses and other particles in the room. The filter then pushes clean air out through the other side.
You may think filtration methods would be less effective with smaller particles such as aerosols. However, this is not true. Aerosols are trapped with even higher efficiency.
Disinfection is an option for higher-risk spaces such as cafeterias, schools, and nursing homes. Disinfection kills the virus but doesn’t physically remove it.
The virus can last in the air from minutes to hours and survive for an hour when floating in aerosols. They gradually decay over time, there may be a fast decay at first, but they are there. And there, they can infect you.
The indicators of good air quality are making sure you have increased your ventilation rate, putting in air filters, adding measures such as carbon monoxide monitors, and making sure a lot of fresh outdoor fresh air is coming inside.
The importance of awareness and equity
Kenneth Martinez

We need access to science-based and proven information regarding risk mitigation and overall infection.
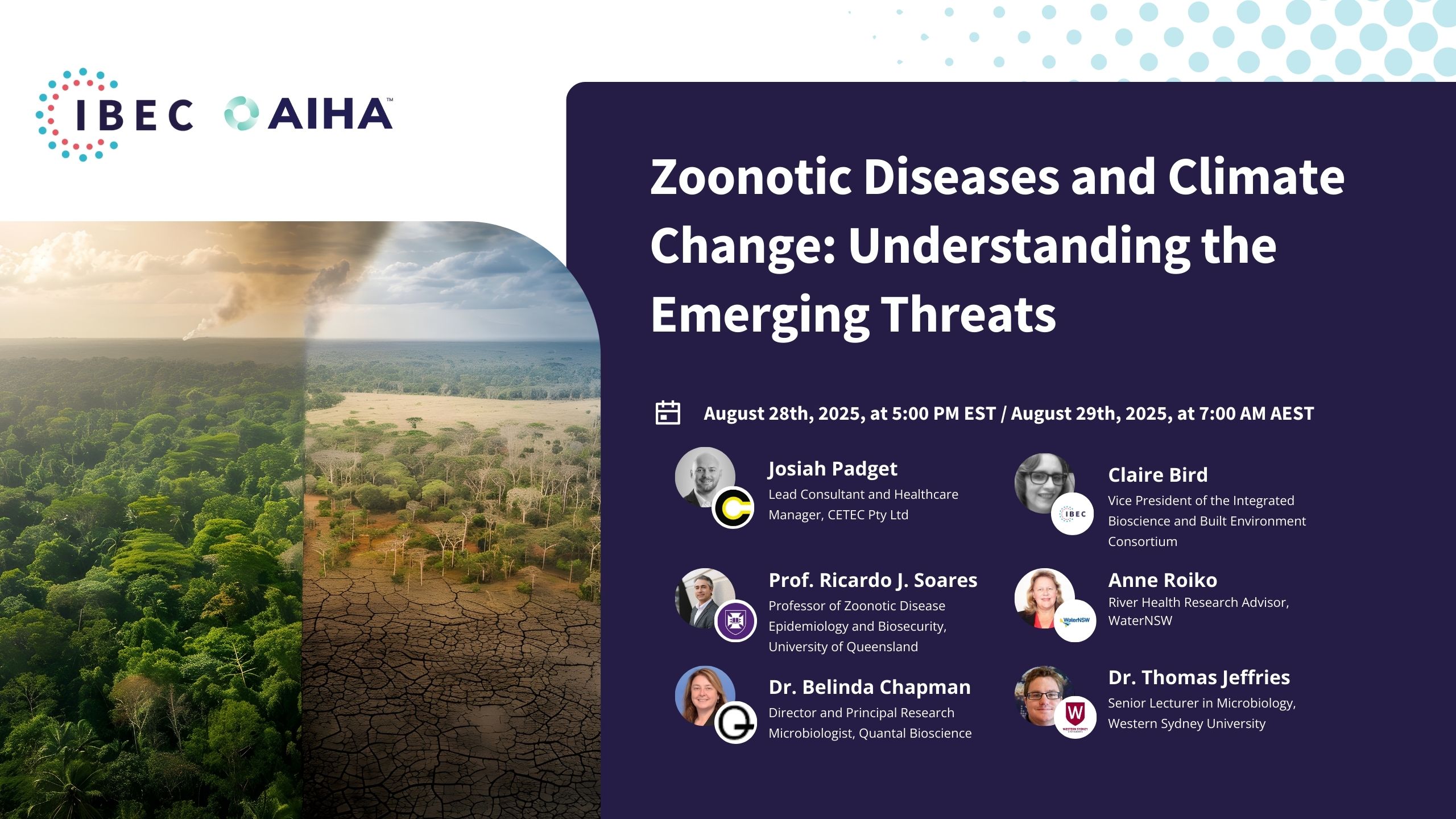
Thus, The Integrated Bioscience and Built Environment Consortium (I.B.E.C.) and the American Industrial Hygiene Association (AIHA) have compiled a collection of digested resources on these specific topics, such as awareness and understanding of environmental mitigation strategies. Pledge to Commit to C.A.R.E. today!
To assess the risk of highly transmissible diseases such as COVID-19, you should consider the 4DS – density, duration, distance, and dilution.
When you walk into a place and want to assess your risk of getting infected, consider:
- How many people are in the room.
- How much time will you be staying
- If people in are practicing social distancing
- If there are efforts to dilute the virus particles in the space such as proper ventilation or filtration.
Dilution, in particular, serves two purposes – manage pollution and provide free cooling and heating. However, when we increase the amount of indoor air, it increases energy costs, so you need to consider the impact on energy costs.
In terms of filtration, The American Society of Heating, Refrigerating and Air-Conditioning Engineers (ASHRAE) currently recommends increasing your filtration rates to a MERV 13. This gives you an approximately 85% efficiency and removal of various sizes of particles.
There is a problem with filtration because as you increase filtration efficiency, you also create greater resistance to air movement, making your system motor components work harder. So we would refer you to the Associated Professional Engineering Consultant (APEC) to understand if that will work for you.
Two tried, and accurate supplemental air cleaning technologies are portable air cleaner/air purifiers (HEPA. filters) and Germicidal Ultraviolet Radiation (GUV). With GUV, implementation and maintenance issues include potential health effects if not installed correctly.
To control the risk of COVID-19 infection, the best thing you can do is go back to what we know does work – filtration.
The importance of schools
Tracy Enger

The United States Environmental Protection Agency (EPA) has been working on indoor air quality since 1988. Their focus on schools began in 1994 With the introduction of our indoor air quality tools for schools kit in response to a U.S. Government Accountability Office (G.A.O.).
People need to understand that where students learn is just as important as what they learn. We have unique challenges when addressing indoor air quality in schools because of the vulnerable populations there.
Children are physiologically different; they breathe deeper and faster and are, in general, more vulnerable and susceptible to many exposures.
The COVID-19 pandemic has changed the need for better air quality, and Tracy Enger explains it with three A’s: Awareness, Ability, and Action.
We see more schools putting our guidance into action, and we want to come out of this crisis with ongoing and lasting outcomes and commitments.
Related resources:
AIHA University.
Back to work safely.
Commit to C.A.R.E.
AIRAH’s Indoor Air Quality Assembly.
Virtual Event Transcript – Let’s Clear the Air: An OSTP Discussion on COVID and Clean Indoor Air.
National COVID-19 Preparedness Plan.
5 Economic Changes Caused By The Pandemic.
COVID 19, Crisis Response, Mental Fatigue & Resilience.
Beyond COVID-19.
Why Did It Take So Long To Accept COVID Is Airborne?
Top Guidelines To Follow In The COVID-19 Era.
Related Blogposts
How Climate Change is Propelling the Spread of Infectious Disease
By Stephane Bilodeau, Eng., Ph.D., FEC, Chief Science Officer at IBECClimate change is not only an ecological crisis; it fundamentally alters public health dynamics worldwide…
IBEC Statement on the Quarantine of Cargo Ship in Argentina Due to Suspected Mpox Case
The recent news regarding the quarantine of a cargo ship near Argentina’s Rosario Port due to a suspected case of mpox underscores the continued global…
Interdisciplinary Collaboration in Environmental Science: Pioneering Health Solutions with IBEC’s New CSO
The Integrated Bioscience and Built Environment Consortium (IBEC) proudly introduces its new Chief Scientific Officer (CSO), Stephane Bilodeau. Bringing over 25 years of diverse experience…
Navigating the Rise of Bacterial Pneumonia: Insights and Precautions
Navigating the Rise of Bacterial Pneumonia: Insights and Precautions As winter’s chill sets in, health professionals and organizations brace for the annual uptick in respiratory…
New COVID-19 Variant JN.1 Raises in the United States
JN.1 is a highly contagious, fast-spreading subvariant of omicron that has become the dominant strain in the country. According to data from the Centers for…
Pioneering Steps to Control Infectious Aerosols: Dr. Claire Bird Offers Expert Insight on ASHRAE’s New Draft Standard
As we navigate through the challenges posed by the COVID-19 pandemic and other airborne diseases, there is a dire need to implement measures that will…
IBEC Takes the Lead in Developing a Framework for Reducing Indoor Pathogen Transmission
Dear IBEC Partners and Supporters, As we continue to navigate the ongoing threat of airborne pathogens transmission in our shared indoor communities, it’s more important…
New Commit To C.A.R.E. Resources Deliver Innovative Indoor Air Quality Solutions for Safer Workplaces
The Commit to C.A.R.E initiative The Integrated Bioscience and Built Environment Consortium (IBEC) and The American Industrial Hygiene Association (AIHA), two leading organizations committed to…
Staying Ahead of Severe GAS Infections and Other Secondary Bacterial Infections
Severe Group A Streptococcal (GAS) infections, including invasive disease (iGAS), can lead to life-threatening illness and death. CDC is looking into an increase in…
Industry Leader L’Oréal Pledges to Support Commit to C.A.R.E.
Industry Leader L’Oréal Pledges to Support Commit to C.A.R.E. With health experts warning of the triple threat of the continued spread of new COVID-19…