Watch this recording for a dedicated discussion on indoor air quality (IAQ) and its impact on infectious disease transmission in the built environment
CLEAN Lessons Learned
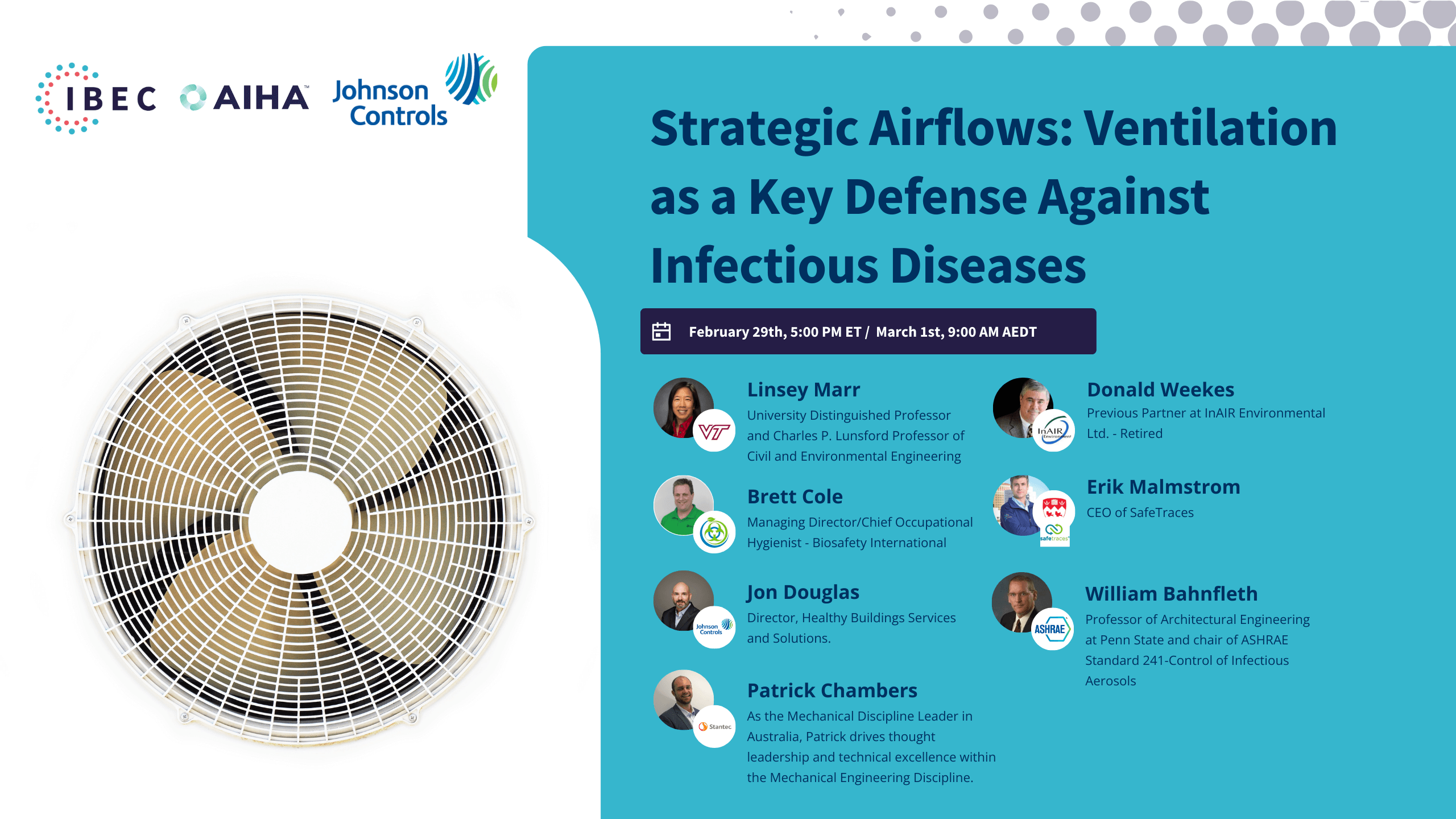
Strategic Airflows
Ventilation as a Key Defense Against Infectious Diseases
In this session, we deep-dived the pivotal role of ventilation in maintaining healthy indoor environments and discussed its effectiveness as a tool against spreading infectious diseases. By delving into the nuances of effective ventilation systems, we provided a comprehensive understanding of how these systems can be used strategically in various settings to mitigate the risk of infectious disease transmission.
IBEC and the Commit 2 C.A.R.E program focus on the 4D’s to reduce the spread of airborne infectious disease. These are Distance, Density, Duration, and Dilution. Ventilation dilutes airborne contaminants, including aerosols, the particles that carry a pathogen from an infected to an uninfected person. Adjusting ventilation in our indoor spaces can reduce the long-range spread of airborne disease. This is an important control measure as we face an increasingly diverse range of respiratory infections with high transmissibility carried through the air and our air conditioning systems.
The session featured a panel of distinguished experts from Virginia Tech University, InAIR Environmental, SafeTraces, Inc., Johnson Controls, and The American Society of Heating, Refrigerating, and Air-Conditioning Engineers (ASHRAE). These panelists brought a wealth of knowledge in air quality, bioengineering, and occupational hygiene, and their insights were invaluable in guiding our discussions and strategies toward healthier, safer environments.
- Importance of Ventilation: Ventilation plays a crucial role in controlling indoor contaminant levels, including infectious aerosols, emphasizing the need for a broad definition of ventilation that includes not just outdoor air but also engineering controls.
- Engineering Controls for Infectious Diseases: The effective management of infectious diseases indoors requires a combination of strategies, including filtration, germicidal UV, and other air cleaning technologies, highlighting the complexity of achieving optimal indoor air quality.
- Research, Standards, and Regulation Gaps: The COVID-19 pandemic revealed significant gaps in research, standards, and regulations related to infectious disease control in buildings, underscoring the need for urgent advancements in these areas.
- Multi-dimensional Risk Management: Effective infectious disease control requires a multi-layered approach, incorporating engineering controls, personal protective equipment, and behavioral changes, among others.
- Development of ASHRAE Standard 241: This standard aims to establish minimum requirements for the control of infectious aerosols across all building types and throughout the building lifecycle, indicating a move towards comprehensive standards for infection control.
- Equivalence of Clean Air Flow: The concept of equivalent clean airflow is introduced as a more flexible and potentially energy-efficient alternative to specifying minimum outdoor airflow rates, allowing for the use of air cleaners and other technologies.
- Adaptation of Buildings: The challenge of adapting existing buildings to meet new ventilation and air cleaning standards was discussed, highlighting the need for creative solutions and the potential difficulty of retrofitting older infrastructure.
- Portable Air Cleaners and Maintenance Concerns: The use of portable air cleaners has increased, but concerns about their long-term effectiveness, maintenance, and the potential for them to be moved or turned off were raised, suggesting a preference for more permanent, integrated solutions.
- Collaboration with Public Health Agencies: The necessity of bridging the gap between engineering solutions and public health policies was emphasized, indicating a need for collaboration to implement effective controls for infectious diseases in public spaces.
- Emergency Preparedness and Response: The discussions reflected on the reactive measures taken during the COVID-19 pandemic and highlighted the importance of having preparedness plans that include engineering controls as part of a broader emergency response strategy to infectious disease outbreaks.
Brett Cole
Managing Director/Chief Occupational Hygienist - Biosafety International
Brett is Managing Director/Chief Occupational Hygienist – Biosafety International/Member of Indoor Air Quality Association of Australia and Education & Training Committee (ETC) of Association for Biosafety for Australia and New Zealand.
Brett has been working in contamination control/hygiene in the High containment, Life Sciences, Healthcare, and Food/Beverage Market for over 20 years. His formal qualifications are in Environmental Microbiology & Chemistry and later in Occupational Hygiene and Toxicology.
His experience has been in Academic microbiological research, Medical device High-Level Disinfection, Engineering controls for contamination control in the built environment, materials handling, infectious and contaminated waste and facility microbial testing, decontamination, and remediation.
He has worked in Australia, New Zealand, Europe, North America, and Asia Pacific on many contamination projects from Beta-lactam site remediation for the Pfizer Vaccine Development, Research Animal Facility Infection, Pharmaceutical decontamination, Mold Infestation, Biological Contaminated Building decontamination.
In 2018, Brett wrote and presented the training material for the Safe use of Biological Safety Cabinets for the International Federation of Biosafety Associations (IFBA) and is a Certified Biorisk and Biowaste Professional with IFBA. He is also the lead Biosafety & Biosecurity Consultant to the PNG HIV and Malaria High Containment Facility in Port Moresby.
During the COVID-19 Pandemic, he has worked with two Federal Government Task Forces on PPE and Ventilators, IAQA Guidelines for Validation of Virally contaminated buildings as well as being the first International Contributor to a Technical Working Group on Decontamination for COVID-19 and a founding Contributor of IBEC.

Donald Weekes
Previous Partner at InAIR Environmental Ltd. - Retired
Mr. Weekes has over forty-eight (48) years of comprehensive consultation expertise and project experience in the implementation and management of inspections for hazardous materials in numerous buildings throughout Canada and the United States including universities, colleges, governmental offices, and commercial and residential buildings. During Mr. Weekes’ career, he has served in numerous senior management positions in both the consulting and insurance industries. He has provided consultation services, including health and safety audits and environmental air sampling, to a wide variety of facilities in the utility, chemical, petroleum, petrochemical, and pharmaceutical industries. He has also worked with numerous governmental entities at local, state, provincial, and federal levels.
As a Certified Industrial Hygienist (CIH) and a Certified Safety Professional (CSP), Mr. Weekes has served as an environmental health and safety professional for various international corporations. He has worked as a consultant for firms in the United States, Canada, Great Britain, Germany, France, Finland, and Switzerland.

Linsey Marr
University Distinguished Professor and Charles P. Lunsford Professor of Civil and Environmental Engineering
Professor of Civil and Environmental Engineering at a major research university whose environmental engineering program is ranked in the top 10.
Her experience includes managing scientific research, teaching graduate and undergraduate courses, advising MS and Ph.D. dissertation research, publishing in the scientific peer-reviewed literature, giving technical presentations, obtaining grants for research, reviewing research proposals and papers for scientific journals, and serving on a Board and committees for the National Academies of Sciences, Engineering, and Medicine.
Dr Marr has over 20 years of experience in research on atmospheric chemistry and transport, air quality engineering, and bioaerosols, including laboratory, field, and modeling experiments.

Jon Douglas
Director, Healthy Buildings Services and Solutions.
Jon Douglas is the Director of Healthy Buildings Services and Solutions at Johnson Controls. Throughout his 30-year career in the HVAC&R industry, he has established a reputation as an innovator. During the COVID outbreak, Jon studied the fundamentals of infection control in buildings and became JCI’s leading technical expert in clean air strategies for buildings. Jon is an active member of ASHRAE 241 and 62.1 Standards committees.

William Bahnfleth, PhD, PE, FASHRAE, FASME, FISIAQ
Professor of Architectural Engineering at Penn State and chair of ASHRAE Standard 241-Control of Infectious Aerosols
William Bahnfleth is a professor of architectural engineering at The Pennsylvania State University. He holds a PhD in mechanical engineering from the University of Illinois at Urbana-Champaign and is a Registered Professional Engineer. He is a Fellow of ASHRAE, ASME, and ISIAQ. Dr. Bahnfleth’s primary research interest is how to deliver high indoor air quality sustainably, with a focus on control of infectious aerosols. He has led experimental and analytical studies of the performance of germicidal ultraviolet disinfection systems in both airstream disinfection and upper room implementations. Dr. Bahnfleth is a past president of ASHRAE and current vice-president of the Indoor Environmental Quality Global Alliance. He chaired the ASHRAE Epidemic Task Force and is the current chair of the ASHRAE Environmental Health Committee and ASHRAE standard project committee 241 Control of Infectious Aerosols.

Patrick Chambers
Australian Discipline Leader, Mechanical Project Engineer, Associate Director at Stantec
As the Mechanical Discipline Leader in Australia, Patrick drives thought leadership and technical excellence within the Mechanical Engineering Discipline. His diverse background in mechanical engineering, academic research and contracting experience enables him to blend practicality and innovation into technical problem solving.
He works extensively within the healthcare sector and is experienced in the delivery of hospital projects of varying sizes, from minor refurbishments to major redevelopments.
Throughout his career, Patrick has kept a close association with research institutions, including the undertaking of post-graduate activities and the funding of industry-led research projects in conjunction with tertiary academia, particularly on the subject of indoor air quality and airborne infection control.

Erik Malmstrom
CEO of SafeTraces
Erik Malmstrom is the CEO of SafeTraces, a market leader in technology-enabled testing, verification, and commissioning of HVAC and air cleaning systems to optimize indoor air quality and energy efficiency. Erik received his undergraduate degree from the University of Pennsylvania and a joint MBA-MPP from Harvard Business and Kennedy Schools, and is a combat veteran and graduate of US Army Ranger and Airborne School.
Strategic Airflows: Ventilation as a Key Defense Against Infectious Diseases
SUMMARY KEYWORDS
ventilation, building, aerosols, air, standards, ashrae, control, ventilation rates, rate, people, pathogens, infection control, pandemic, uv, talk, outdoor air, problem, air cleaners, solution, clean air
SPEAKERS:
Linsey Marr, Jon Douglas, Patrick Chambers, Erik Malmstrom, William Bahnfleth.
Kenneth Martinez 0:02
Good evening to those in the United States time zone, and for our international visitors, good morning or good afternoon, whichever applies. My name is Kenneth Martinez, and as the current president of the Integrated Bioscience in the Built Environment Consortium, or IBEC, it is my pleasure to welcome our moderators, panelists, and all attendees to this third event in the Lessons Learned series. Today, we’re focusing on strategic airflows and ventilation as a key defense against infectious diseases. This event is co-sponsored by the American Industrial Hygiene Association, IBEC, and Johnson Controls. I am confident that you will learn a lot and have questions for our panelists tonight. Our first speaker is unable to attend in person, so we will begin with a pre-recorded video of Dr. Linsey Marr from Virginia Tech University. She will engage in a discussion with Stephane Bilodeau, the current IBEC Chief Science Officer, in a town hall format. Following this, we will proceed with a moderated session for the remaining panelists. Our moderators for the upcoming session are Don Weeks and Brett Cole, who will introduce the panelists individually. Enjoy tonight’s event, and please note that it is recorded. If you’re unable to view it live or wish to refer friends to it, visit the weareibec.org website, where you can find recordings of the event. Please start the video.
Stephane Bilodeau 1:38
Today, we are absolutely delighted to welcome Linsey Marr, the distinguished Charles P. Lunsford Professor of Civil and Environmental Engineering at Virginia Tech, to our CLEAN Lessons Learned series. Welcome, Linsey. Let me first provide our attendees with some insights into your remarkable professional background. You began your engineering studies at Harvard University, graduating summa cum laude—a significant achievement from the outset. You then pursued your PhD at the University of California at Berkeley, followed by postdoctoral research at MIT, before joining Virginia Tech in 2003. Over the years, you have received numerous awards and fellowships, notably from the International Society for Indoor Air Quality and Climate in 2018, the American Association for Aerosol Research in 2021, and the American Geophysical Union in 2022. More recently, in 2023, just a few months ago, you were elected to the National Academy of Engineering and named a MacArthur Fellow by the prestigious MacArthur Foundation. Congratulations, by the way. Additionally, from the onset of the COVID-19 pandemic, you have not only researched airborne disease transmission of SARS-CoV-2 but also participated in many initiatives to help protect people, notably with the Lancet COVID-19 Commission Taskforce on Safe Work, Safe School, and Safe Travel. Today, you will discuss some of the task force’s recommendations and delve further into ventilation for maintaining a healthy indoor environment. We are honored to have you, Linsey, as our keynote speaker today. Without further ado, the floor is yours.
Dr. Linsey Marr 3:40
Thank you very much for the introduction. I welcome those interested in this subject. I’m going to go ahead and share my screen. Today, I’m going to talk about new recommendations for ventilation in buildings, because things have changed over the past four years. We’re going to start by looking at this example lecture hall or classroom. It’s about 25 feet by 40 feet in area, it has 10-foot-high ceilings, and let’s say there are 35 people in there. Now, pre-pandemic, the ASHRAE recommended ventilation rate would be 500 cubic feet per minute of outside air, and this would correspond to 13 cubic feet per minute per person. We often hear about air change rates and ventilation rates discussed in terms of air changes per hour. We can use this information to calculate the number of air changes per hour, to figure out how long it would take to clear the air, replace the air that’s in there with outdoor air. And so, to calculate that, we take the ventilation rate of 500 cubic feet per minute, divided by the volume of the room, which is 10,000 cubic feet, and then multiply it by a conversion factor, and so we get three air changes per hour. That means that every 20 minutes, most of the air is removed and replaced by cleaner outdoor air.
Why does this matter? We know that for viruses that transmit through the air, ventilation helps by diluting virus that’s in the air, leading to less exposure of the virus for those who are in the room. This has been shown in several real-world experiments. There was a study done by Don Milton’s group, looking at dormitories, and they had a dormitory with low ventilation and one with high ventilation. They found lower rates of acute respiratory infection in the dorm that had high ventilation. There’s also been a human challenge study involving influenza, where a participant was deliberately infected with the flu, and then exposed to many susceptible people under different conditions to see how much transmission would occur. In this experiment, there was a lot less transmission than expected. They think because the ventilation rate in the rooms where they held the study was higher than they had planned for. And then finally, during the SARS-CoV-2 pandemic, the COVID-19 pandemic, there was a large study in Italy of schools, and they found that there was an 80% lower risk of SARS-CoV-2 infection in schools that had high ventilation rates. The figure on the right shows the results from that study in Italy. On the x-axis, it shows ventilation rate per person in liters per second per student, and on the y-axis, it shows the relative risk of outbreaks occurring. So, you can see that at low ventilation rates, where they had no mechanical ventilation in that gray box, the relative risk was fairly high. And as you increase to higher ventilation rates along the x-axis, where I show a breakpoint at 10 liters per second per student, which corresponds to 21 cubic feet per minute per student, you can see that the relative risk is much lower at those higher ventilation rates.
Recently, there was a review published by Cy Wu’s group, and they surveyed 93 studies where SARS-CoV-2 had been measured in the air, and they knew something about ventilation rates. They found that the amount of SARS-CoV-2 in the air was negatively correlated with the air change rate and with air changes per hour. This figure shows, along the x-axis, the number of air changes per hour in each of those spaces, in bins of zero to four, four to eight, eight to twelve, twelve to sixteen, and greater than sixteen air changes per hour. And below that indicates the number of measurements from those spaces that fall in that category. And the y-axis shows the concentration of SARS-CoV-2 gene copies, the RNA of the virus, per liter of air. And you can see that the highest concentrations of virus in the air are found at those low air changes per hour of zero to four. And as the number of air changes per hour increases, there’s less virus that’s found in the air.
In 2022, the Lancet COVID-19 Commission Task Force on Safe Work, Safe School, and Safe Travel, which is led by Joe Allen at Harvard, proposed non-infectious air delivery rates, which is like a clean air delivery rate or ventilation rate, in essence, for reducing exposure to airborne respiratory infectious diseases. This was motivated by the fact that current ventilation targets were too low, and that improving on these minimums could lead to big gains. We found that there was general coalescence around desired targets across different organizations and research groups, across different metrics also, which I’ll discuss now. The main take-home message from this report is this table, where we proposed non-infectious air delivery rates or targets for reducing exposure or reducing the risk of transmission. We categorize these as good, better, and best. And right now, I’m highlighting this in terms of air changes per hour. ACH E stands for equivalent, which we’ll talk about. There are different ways of getting clean non-infectious air, and we recommended four air changes per hour for good ventilation, six for better, and greater than six for best. This is in terms of volumetric flow rate per volume. There are other ways to talk about and measure ventilation in buildings. The second way is thinking about it in terms of volumetric flow rate per person. This is cubic feet per minute per person, or liters per second per person. And there, you can see that we suggest that good ventilation could be achieved at 21 cubic feet per minute per person. Now, recall in that initial classroom example, the rate was 13. So it was not quite good. And then up to a level of greater than 30 cubic feet per minute per person for the best case scenario. The third way of thinking about the ventilation rate is in terms of the flow rate per area of the floor. And here, you can see that a good level would be 0.75 cubic feet per minute per square foot, plus on top of the ASHRAE minimum. And the best case would be if you could get greater than one cubic foot per minute per square foot on top of the ASHRAE minimum.
Now, good ventilation is important not only for reducing the risk of transmission of airborne diseases but it also has many other benefits. The Lancet Commission also put out a report on designing infectious disease resilience into school buildings through improvements to ventilation and air cleaning. And in this, we review the literature on the topic. And we have a table in there that shows that if you have good ventilation, that is correlated with higher test scores on reading, math, and science exams, improved cognitive function, and is negatively correlated with respiratory symptoms. So if you have higher ventilation, we see lower respiratory symptoms, reduced asthma symptoms, and reduced absenteeism.
Now, the CDC, the U.S. Centers for Disease Control, now recommends aiming for at least five air changes per hour in a space. So, here in this table, I’m showing how that corresponds to the other metrics. So, if we start out in red with five air changes per hour, and we want to think about that in the other metrics, per person and per area, we need to first of all take that five air changes per hour. If you look in the lower right box, I have the equation that shows you how to convert. You take the air changes per hour, multiply by the area and height of the room, and divide by that conversion factor of 60 minutes per hour. So, I take five air changes per hour, multiply by 1,000 square feet and 10 feet for the ceiling height, divided by 60. And I get a total airflow rate of 833 cubic feet per minute. If I divide that by the 35 people in the room, I now have 23.8 cubic feet per minute per person. Or, if I divide the 833 by 1,000 square feet, the area of the room, I have 0.83 cubic feet per minute per square foot.
Last year, ASHRAE came out with a new standard, 241, for control of infectious aerosols. They talk about it in terms of minimum equivalent clean air flow per person. And equivalent clean air flow is the same thing as the non-infectious air delivery rate that we discussed in the Lancet COVID-19 task force report. And so, for a classroom, they recommend now 40 cubic feet per minute per person in a classroom with 35 people. And so, if we take that 40 and multiply by 35 people, we get a total flow rate of 1,400 cubic feet per minute. And again, I can take the equation shown on the right-hand side and go from total cubic feet per minute, divided by the area and height of the room, multiplied by that conversion factor of 60, to get the number of air changes per hour. So, the 40 cubic feet per minute per person, shown in red in that table at the bottom, corresponds to an air change rate of 8.4, rather than three in the initial example, and an area per area rate of 1.4 cubic feet per minute per square foot.
So, finally, if we come back to that example I had at the beginning, those, it showed numbers for pre-pandemic recommendations, the new ASHRAE recommended ventilation rate corresponds to instead of 500 cubic feet per minute of outside air, it’s 1,400 cubic feet per minute of outside air, corresponding to 40 cubic feet per minute per person. And instead of three air changes per hour, now we’re looking at 8.4 air changes per hour. Now, the equivalent clean air flow or non-infectious air, you can achieve that through a few different ways. The first is ventilation with outdoor air. That’s shown in the picture where the windows are open, and there are fans on. The second way you can do that is through filtering the air, either with a portable air cleaner, shown in the lower right corner of that classroom, or through filters, good quality filters in the central HVAC system. Those will physically remove pathogens from the air. And the third way you can achieve that is through disinfection. A well-established way to do that is through UV germicidal irradiation, or UVGI, which here in the figure, number three, is shown aimed at the ceiling in order to prevent exposing people to UV radiation. And that UV is known to kill off or inactivate pathogens that are in the air.
So, in conclusion, first of all, you should follow the requirements for your building. There are specialized types of buildings, for example, hospitals, where there are already existing standards, even from before the pandemic. And those are what you should follow. The second point is that there are three ways to measure the non-infectious air delivery rate, the NADR, or the equivalent clean air flow rate. And that is, first of all, on a per volume basis, which gives you air changes per hour. The second is on a per person basis. And the third is on a per area basis. These new Lancet recommendations, WHO, and CDC guidelines, and ASHRAE 241 are higher than previous standards. And they produce similar results for typical spaces. There’s a couple of special cases. First of all, in very crowded spaces, the per person recommendations, cubic feet per minute per person, may be best. And in spaces with high ceilings, the per person and area recommendations may be best, rather than air changes per hour. Thank you very much for your attention.
Stephane Bilodeau 16:23
Thank you, Linsey, for this excellent summary and the vital recommendations for a healthier indoor environment. I have a few questions and would like your feedback on several points you’ve made, particularly regarding the standards and their effectiveness in preventing disease transmission, with a focus on long-range transmission. To be more direct, from your perspective, what are the blind spots in current ventilation and filtration standards in this context?
Dr. Linsey Marr 16:58
Yes, that’s an excellent question. I’m pleased you brought up long-range transmission because the existing standards are primarily aimed at reducing what we term long-range transmission, or transmission at a distance greater than three to six feet, essentially across the room scenarios where you happen to be in the same room with an infected person. However, what these standards do not address effectively is the risk reduction during close, face-to-face interactions. For example, if you’re sitting next to or directly in front of someone who is coughing or talking, and they happen to be infected, in such cases, one needs to employ additional strategies like distancing or masks. These standards were not designed to mitigate risks associated with close-range interactions through ventilation and filtration alone. Therefore, they apply to the air in the entire space, rather than addressing potential pockets of higher virus concentration that may occur when you are in close proximity to an infected individual.
Stephane Bilodeau 18:04
That’s a great point. These measures are indeed valuable tools in our toolbox, but they must be combined with other protections and measures. Excellent observation. On that note, you’ve mentioned metrics, but which metrics are commonly used that could help assess ventilation more efficiently and effectively? How can we determine the effectiveness of ventilation and more?
Dr. Linsey Marr 18:25
I discussed three different metrics used to describe ventilation: air changes per hour, cubic feet per minute per person, or cubic feet per minute per area of the room. These are not easily known by the average person; typically, a facilities or building manager would be aware of these values. A fourth tool that we can use is carbon dioxide measurements. There are small portable sensors that some people can use and carry around with them. You can look at the carbon dioxide level—carbon dioxide is in our exhaled breath and is removed with good ventilation—as another indicator of ventilation. Our report and some of the ASHRAE Standards, as well as other standards I’ve mentioned, address these. Additionally, I want to note that those three different metrics I’ve discussed here might lead people to wonder, “Which one should I use?” For an average space, all three will give similar results. Differences emerge in extremely crowded environments, like a packed bar, or spaces with high ceilings, such as a big box store or a basketball arena. In those cases, you may want to use the per person or per area ventilation rates more. Another special case is where you have low occupancy, maybe only two people in a room. If one of them is infected, then you would need to take some other considerations into account.
Stephane Bilodeau 20:12
Those are excellent points. Each is important, with some being more suited to specific, special situations. Indeed, understanding the metrics first is crucial to grasp what you’re dealing with. Great point, thank you. I just want to express my sincere appreciation for your participation in this CLEAN Lessons Learned series and for your vital insights on ventilation as a key defense against infectious diseases. We are truly grateful for your contribution here. Thank you.
Dr. Linsey Marr 20:47
Thank you very much.
Stephane Bilodeau 20:49
Back to you on the mainstage.
Donald Weekes 21:07
Hello, I’m Donald Weekes, and I have the privilege of moderating this session alongside my co-moderator, Brett Cole. Our first speaker is Jon Douglas. He will be giving us a presentation. Let me just pull up his resume. He is the Director of Healthy Building Services and Solutions at Johnson Controls. Throughout his 30-year career in the HVAC industry, he has established a reputation as an innovator, particularly during the COVID outbreak. Jon studied the fundamentals of infection control in buildings and became JCI’s leading technical expert in clean air strategies for buildings. Jon is an active member of the ASHRAE 241 and 62.1 Standards Committees. Jon.
Jon Douglas 22:05
Okay, what I’m going to do today is take a lot of the information that Linsey presented about how you can clean the air and then add an energy efficiency context to it. This way, we can explore the options for sustainably cleaning the indoor air and managing infection risk. First, let’s review. There are basically three ways we can clean the air. The first one is outside air ventilation. We’ve talked about this; it’s the idea of bringing outside air into the building, which is really good at getting rid of gas-based pollutants but doesn’t do much for removing particles. And, as we mentioned before, it’s very effective at removing those respiratory droplets by diluting the air. The second tool we have is filtration. Filtration is really good at getting rid of particles and is also effective at eliminating pathogens, making it another tool for managing infection risk in buildings. The final method is UVC disinfection, which doesn’t do much for gas-phase pollutants or particles but does a great job on the pathogens.
In developing standards like ASHRAE 241, we introduced a common metric called the equivalent clean air flow, which associates the pathogen-reducing potential of each of these technologies. This allows us to compare the different technologies to achieve the same amount of infection risk reduction.
I’m going to spend a lot of my time talking about a field study we conducted at MIT a few years ago. It was a collaboration with Dr. Martin Van Zandt in the chemical engineering department and the facilities folks at MIT. When schools were in session, we added air quality sensors, which are these boxes here; you can see one in the room right here. From the facilities folks, we were able to collect Building Automation System data on airflows, energy consumption data, and, coolly, we were able to measure occupancy data in the classroom. We had graduate students go out and actually measure the number of students in each class, giving us real occupancy data.
With this information, we began working on how to validate models for infection risk. A key assumption in many of the infection risk models is the well-mixed assumption. We thought we could use the data we collected to validate this assumption. We looked at CO2 data, as many know, CO2 is used as a tracer gas. We often use it for demand control ventilation and measuring. People generate CO2, and bringing in outside air removes it. By applying a mass balance, we can determine the ventilation rate. So, if you know the ventilation and CO2 levels, and the number of people, if you have three variables and know two, you can calculate the other one.
What we did was, based on the CO2 readings and the ventilation rate, we estimated the number of people in a room, shown by these green lines. You can see the first top one here is a classroom, and the bottom one is an office space. The black dots represent the measured occupancy, the actual occupancy. In the classroom, we did a pretty good job of predicting occupancy; the dots align well with the peak measurements from the CO2 readings and airflow. This chart is a zoom-in of that one hour, and you can see we’re quite close in estimating the peak occupancy. In the office, although the occupancy isn’t a step change but more variable, we’re capturing the variation in occupancy quite well. Based on this, we feel that, using a single CO2 sensor in a room, the well-mixed assumption in a typical operating building is reasonable.
Next, I’ll show some example data we collected. On top, we have data from our IQ sensors, showing CO2 measurements for several classrooms. On the bottom, we have data from the building automation system. You can see the outside airflow rate is pretty constant. MIT’s strategy at the time was to maximize outside air ventilation, running roughly at about six air changes per hour of outside air for classrooms and about four for office spaces, then turning off at night when nobody’s there. We see a real opportunity for energy savings on weekends and holidays when nobody is in the space.
Zooming in on one day, you can see the CO2 signal spikes with different classes. For example, this orange one has only one big class that day, and then it’s unoccupied the rest of the time. Providing ventilation to these corners means spending a lot of money providing outside air when there’s nobody really in the space, presenting an opportunity for energy savings.
This last slide summarizes what we did. We used a Wells-Riley based infection risk model to calculate the infection risk of different mitigation strategies. The horizontal axis is the transmission rate, and the vertical axis is the energy cost in dollars per day. The blue box is the baseline case where we’re providing maximum outside air ventilation. The transmission rates might be a bit confusing, so I added a reference line equivalent to 40 cfm per person, as recommended by ASHRAE 241.
Looking at the baseline case, if we apply a schedule to ventilate only during operating hours and shut things down at night and on weekends, we cut energy consumption in half, though the infection transmission rate increased slightly due to imperfect scheduling. Reducing to standard ASHRAE 62.1 ventilation rates further reduces energy consumption but increases the transmission rate since ventilation has decreased further. Demand control ventilation adjusts ventilation based on occupancy, leading to more energy savings but at the cost of a higher transmission rate.
What are cost-effective or energy-efficient ways to approach the ASHRAE 241 line? Adding in-zone filtration or a far UV fixture significantly reduces transmission rates with a minimal increase in energy costs. Transmission control ventilation, a variation on demand control that considers occupancy differently, and using everything but the kitchen sink, like transmission control ventilation and far UV, can lead to an 87% energy reduction from the baseline and a 30% decrease in transmission risk.
Before I conclude, it’s important to highlight that systems for managing infection risk are only effective if they’re working, underscoring the importance of monitoring. An example from a hotel IQ audit shows the impact of a system failure on CO2 levels and the swift resolution once identified, emphasizing the necessity of monitoring clean air systems.
Finally, a few pointers: start with providing ASHRAE 62.1 ventilation for gas-based pollutants and pathogen management, then move to filtration as the most cost-effective means for reducing pathogens and removing PM2.5. End with UVC disinfection for high disinfection rates. That concludes my talk.
Brett Cole 33:33
Hello, everybody. My name is Brett Cole, and I’m co-moderating this session with John Weekes. Thank you to everyone for attending. It’s a great pleasure and honor for me to introduce Patrick Chambers. Patrick is a fellow Australian like myself, and he’s the Australian Discipline Leader, Mechanical Project Engineer, and Associate Director at Stantec. As the Mechanical Discipline Leader in Australia, Patrick drives leadership and technical excellence within the mechanical engineering disciplines. Patrick works extensively within the healthcare sector and is experienced in delivering hospital projects of varying sizes, from minor refurbishments to major redevelopments. Throughout his career, Patrick has maintained a close association with research institutes, including undertaking postgraduate activities and funding of industry-led research projects in conjunction with tertiary academia, particularly concerning indoor air quality and airborne infection control. So, it gives me great pleasure to introduce Patrick Chambers. Welcome, Patrick.
Patrick Chambers 34:38
Thanks, Brett. I appreciate it, mate. I’m just going to share my screen. It might take a few seconds to come up. My presentation today focuses on challenging industry conventions. I often see typical approaches to problems in the industry. I believe there’s a significant solution bias within the construction industry, which might be difficult for an outsider to comprehend. As engineers, we have an obligation to provide buildable solutions, leading us to design solutions around products available in the market. This results in a convoluted supply chain but also, I think, creates an innovation blind spot. We often internalize these solutions as second nature, iterating on them. Innovation sometimes becomes just a slightly different approach to the same solution. However, I feel that, from a first principles perspective, we sometimes fail to adequately define the problem and innovate based on the problem itself.
One of the major conventions in the industry is that good ventilation equals good indoor air quality, and there’s no disputing that bad ventilation equals bad indoor air quality. However, I think we can unpack both sides of this equation with more sophistication than merely stating that the solution to all indoor air quality-related problems is to increase ventilation. For an engineer who designs ventilation systems, ventilation has a very literal interpretation, meaning outside air. It comes from the Latin term “ventilator,” which means to be exposed to the wind. Within the industry, it’s about the quantity of outside air being supplied to a room, not the total supply air. In fact, usually, only about a 20% volumetric percentage of the total supply air would be an outside air component.
So, what constitutes a good ventilation rate is an age-old question. I think we should start with what an acceptable ventilation rate is. Industry standards often discuss acceptable ventilation rates. My own literature review, while it may not be 100% accurate, suggests the industry has converged on 10 liters per second of outside air per person as an acceptable ventilation rate, aligning with some figures Lindsay presented.
The indoor air quality side of the equation is also fascinating. When describing indoor air quality problems to those with little background, I ensure to compartmentalize it into one of three different types of problems: particles, which pose a health risk when inhaled; chemistry; or microbes and pathogens, the focus of this session. We have robust strategies for these problems. For particles, we can create a more particle-free environment inside a building than outside, as done in hospitals, labs, and clean rooms. However, our primary mechanism for managing air chemistry inside buildings is dilution with outside air.
The COVID pandemic challenged our approaches to microbes and pathogens, leading practitioners to question the extent of needed strategies. There are many types of microbes and pathogens, and we might not even know about all of them yet. When we talk about viruses, pathogens, and bioaerosols, we’re discussing a very small size distribution of viruses, whereas molds, typically fungi, are quite large and easily filtered out. The release of a bioaerosol comes from people’s respiratory systems; it’s viruses living within us, and when we exhale, the aerosols we release are the mechanism by which viruses move around the air and are inhaled by others.
Lydia Morawska’s studies on what physically comes out of people’s mouths during various respiratory activities revealed that the quantity of particles, or more specifically, the concentration, is significantly higher if people are speaking loudly than if they’re just breathing in and out through their nose. In fact, if people were just breathing through their nose, there’s almost no release of bioaerosols, suggesting a very limited risk profile for the spread of infectious diseases in buildings.
We’ve been modeling typical respiratory activities, setting up simulations that allow us to assess realistic scenarios and do comparative analyses of different ventilation system configurations. One hypothesis we explored early on was that if people are the pollution sources, instead of trying to dilute pollution sources, we should consider exhausting pollution. We found that applying a decentralized localized solution to capture bioaerosols as close as possible to their source significantly reduces the quantity of suspended aerosols.
This finding challenges a primary convention in the industry: that increasing ventilation rate is the best solution. We began to consider centralized versus decentralized filtration. Typically, engineers first look at where to place supply air diffusers for thermal comfort without much consideration for exhaust air locations, which can become the highest risk areas for bioaerosol exposure.
We’ve been investing in innovative technologies, like a mobile robot equipped with various sensors, including audio sensors, to detect areas of high respiratory activity within a building. This helps us identify where risks are highest at any given moment, suggesting the need for dynamic solutions to clear bioaerosols from the room.
One significant question I pose is whether airborne aerosols survive the journey through an air handling system. Different scenarios, such as a typical hotel room with a bulkhead fan coil unit system versus a hospital with extensive ductwork, filtration stages, and environmental changes, require different considerations. If bioaerosols do not make it back to the room in complex systems, then increasing ventilation rates may not significantly impact the non-infectious delivery rate.
This raises a big question in the industry: while many topics are discussed, some major conventions may not be questioned enough. Thank you for your time.
Donald Weekes 46:12
Thank you very much. Our next speaker is Erik Malstrom, he is the CEO of Safe Traces, a market leader in technology-enabled testing, verification, and commissioning of HVAC and air cleaning systems to optimize indoor air quality and energy efficiency. Erik received his undergraduate degree from the University of Pennsylvania and a joint MBA/MPP from Harvard Business and Kennedy Schools. He’s also a combat veteran and a graduate of the US Army Ranger and Airborne School. Erik.
Erik Malstrom 47:03
Thanks so much, Don. And a huge thank you to IBEC and our sponsors for making this event possible and for giving me the opportunity today. Now, I’m going to bring up my slides. Let’s switch to presentation mode. I thoroughly enjoyed Patrick’s presentation, and actually, all the previous comments and presentations from John and Linsey were excellent as well, because they’ve effectively laid the groundwork for my talk, which will focus on lessons from our real-world testing data. Specifically, we’ll look at how ventilation and various strategies that underpin our guidelines and requirements actually perform in practice, based on data from millions of square feet across numerous buildings.
For those unfamiliar with Safe Traces, we are a biotech company based in California, spun out of Lawrence Livermore National Laboratories, part of the US Department of Energy. Over the past decade, we’ve received support from the National Institutes of Health, the FDA, the US Department of Defense, and many other leading research organizations. We’ve developed an aerosol-based challenge agent for HVAC systems, air cleaners, and germicidal UV. This involves a safe, sterile water-based aerosol with DNA tagging, engineered to simulate viruses found in human saliva, using safe materials. We emit it in a volume and particle size distribution similar to human respiratory emissions, especially targeting coughs and sneezes, to understand particle movement, the efficacy of various engineering control strategies in clearing rooms, and preventing the spread of infectious-like particles throughout a building.
Especially over the past year, we’ve seen significant breakthroughs, now having more concrete, verifiable numbers from the CDC and ASHRAE, particularly with the ASHRAE 241 standard, providing a benchmark for measuring building performance. It’s crucial to note that previously, we lacked specific focus on infectious aerosols in indoor air quality and ventilation guidelines, such as ASHRAE 62.1, which explicitly did not address pathogens.
Our approach involves using this DNA-tagged water-based aerosol as a challenge agent dispersed in buildings according to a standardized test protocol. We are recognized as one of the qualified methods for in-place testing requirements of ASHRAE 241. We emit a known concentration of DNA within a room, allowing for a direct correlation to dosage, which is vital for infectious aerosols. Through air sampling, and sometimes surface swabbing, we can determine where particles spread to, how quickly they’re cleared, and then compile all the field data and samples to provide understandable information on airflow, air balance, and equivalent air change and equivalent clean air flow rate, to grasp real-world performance. Additionally, we often incorporate cost, energy, and carbon modeling over our performance testing results to offer a comprehensive view of what actions should be taken in a specific building or area.
Our testing process starts with collecting building and HVAC system information to create modeled performance assumptions. We then apply our aerosol-based testing technology to examine representative areas within the building, analyzing real-world data to identify underperforming or overperforming areas in terms of ventilation relative to CDC and ASHRAE 241 requirements. For underperforming areas, we provide insights on possible causes and recommend remediation strategies. For overperforming areas, we identify opportunities for reducing ventilation to save on costs and energy while maintaining safety. Finally, we document our testing both digitally and through reports, often retesting buildings regularly to ensure sustained performance.
This context sets the stage for discussing how the latest public health guidance compares with our findings, particularly focusing on infection control. As highlighted by previous speakers, infection control is just one aspect of broader indoor air quality concerns. My discussion will delve into how CDC guidelines on ventilation and infection control measures align or differ from our data collected across millions of square feet.
Through our work, we’ve questioned the efficacy of certain CDC guidelines based on real-world performance. For instance, the recommendation to provide at least the minimum outdoor air ventilation per design codes and to increase it beyond code requirements doesn’t necessarily translate to improved infection control outcomes. Our findings suggest the effectiveness of such strategies is highly dependent on the specific building and not universally applicable across all settings.
We’ve observed that strategies like upgrading central HVAC filter efficiency to MERV 13 or higher and using portable or built-in high-efficiency or HEPA fan filtration devices show more consistent effectiveness in real-world scenarios. However, addressing infection control within the broader framework of indoor air quality requires a nuanced approach that takes into account the building’s specific capabilities, financial implications, energy considerations, and practical concerns like noise and maintenance.
In conclusion, the journey toward better indoor air quality and infection control is complex, demanding clear focus, understanding of the building and system capabilities, and a comprehensive strategy that balances health, energy efficiency, and operational considerations. Through our work, we aim to contribute valuable insights and data-driven recommendations to this ongoing endeavor, helping to shape a safer, more efficient approach to managing indoor environments.
Brett Cole 1:05:22
Thank you very much for that introduction, Eric. It’s a privilege to be back. I have the great honor of introducing Professor William Bahnfleth, who is a distinguished figure in the field of architectural engineering at Penn State University and serves as the chair of the ASHRAE Standard 241, which focuses on the control of infectious diseases.
Professor Bahnfleth is a highly esteemed professor of engineering at Pennsylvania State University. He earned his PhD in mechanical engineering from the University of Illinois and is a registered professional engineer. His contributions to the field are recognized through his fellowship in ASHRAE, ASME, and ISIAQ. His research is particularly notable for its emphasis on the energy-efficient control of bioaerosols.Having served as a past president of ASHRAE, he led the ASHRAE Epidemic Task Force and currently chairs both the ASHRAE Environmental Health Committee and the ASHRAE Standard Project Committee 241 for the control of infectious aerosols.
It’s with great anticipation that we give the floor to Bill, looking forward to the insights he will share in his presentation.
William Bahnfleth 1:06:25
Thank you very much. It appears my slides are ready, so let’s proceed. It’s been enlightening to hear everyone’s perspectives on Standard 241, but given the comprehensive technical discussions that have already taken place, I’ve chosen to take a different approach for my segment. I aim to discuss the effectiveness of engineering controls for infectious diseases and highlight the significant needs for research, standards, and regulation in this area.
Today’s discussion encompasses a broad view of ventilation. According to ASHRAE Standard 62.1-2022, ventilation is defined more expansively than just the introduction of outdoor air. It’s about supplying air to a space to control contaminant levels, encompassing outdoor air and engineering controls such as fibrous filtration, germicidal UV, and reactive species air cleaners. It’s crucial to remember that these controls represent just one aspect of a comprehensive strategy for risk management, emphasizing the need for multi-layered approaches.
Reflecting on the COVID-19 pandemic, which continues, it’s clear that we were underprepared across multiple fronts. This lack of readiness has resulted in significant consequences, from a chronic underinvestment in research to the absence of necessary standards and a regulatory framework that ensures the implementation of controls. Moreover, despite the tremendous impact of the pandemic, discussions have often revolved around the potential increase in energy usage of buildings rather than focusing on health. The silver lining, perhaps, is the heightened public awareness of the necessity for action, presenting an opportunity for change.
Addressing research needs, there’s much we know and yet much more to learn. The Wells-Riley model, often used for infection risk modeling, reveals its limitations with increased use. From air distribution research gaps to the effectiveness and safety of air cleaners, the path forward requires comprehensive investigation to develop practical solutions. Additionally, the development of standards needs a paradigm shift. Current standards do not adequately address infection control or resilience, lacking quantitative metrics for the combined effect of controls. Future standards should redefine acceptable indoor air quality to include infection control and resilience, moving towards an equivalent clean air flow basis.
Regarding regulation, there’s a strong case for its necessity. The reality is that without mandates, advanced measures are unlikely to be widely adopted. Learning from the advancement of national minimum energy standards, similar frameworks for indoor air quality could drive significant improvements, necessitating enforcement to ensure compliance.
ASHRAE Standard 241 represents a positive step towards establishing minimum requirements for controlling infectious aerosols, covering the entire building lifecycle. It’s an add-on for infection risk management, not a replacement for existing standards. Its development, driven by the necessity to bridge building science with public health, emphasizes the use of multiple engineering controls without specifying minimum outdoor airflow rates, focusing on equivalent clean air flow.
In conclusion, the intersection of regulation, standards, and research is crucial for enhancing our preparedness and response to infectious diseases within built environments. The urgency for concerted action is clear, requiring a multi-faceted effort to improve public health and safety.
Donald Weekes 1:19:25
Thank you very much to all the speakers, and I appreciate what your presentations have conveyed. We’re now ready for a Q&A session. To participate, please use the chat feature located in the upper right-hand corner, symbolized by linked balloons. You can submit your questions or comments there, and I will distribute them to the individual speakers as best as possible.
To begin, let’s address some topics that have been discussed. A recent topic of interest is the concept of an evidence-based CFM (cubic feet per minute) per person for clean air delivery. This concept seeks a balance between Standard 62.1 and Standard 241, aiming to harmonize energy efficiency and risk management. Ideally, this would align closely with the CDC’s recommended air changes per hour (ACH). To explore this further, I invite any panel members to share their insights or perspectives on calculating the CFM per person for clean air delivery.
William Bahnfleth 1:20:38
Well, Standard 241 is based on the assumptions we made regarding what constitutes acceptable risk and the characteristics of the pathogen, which is COVID-19. If you look around, you can find a space type within the standard, recommending five air changes per hour. Developing a performance path is one of the items on our work plan for the standard. We approved the development of a calculator at our meeting in Chicago in January, which will allow for the manipulation of some parameters to come up with custom targets. However, when this will be completed and how it might be released for use outside of ASHRAE is yet to be determined. You always have the option when considering this as infection risk management mode, which doesn’t occur all the time. If it’s a severe enough circumstance that you should be taking protective action, one, you can put masks on people, which substantially changes the risk, or two, you can reduce occupancy to match the clean air rate that is actually available in a facility.
Donald Weekes 1:21:50
Thank you, Bill. Does anyone else want to address that question? If not, we’ll move on to the next one. Again, if you have something you would like the speakers to respond to, please place your questions in the Q&A section rather than the chat. I will monitor one, not both. Thank you.
Brett Cole 1:22:11
Some questions have been answered along the way, Don, as well. I noticed there has been some correspondence and answers provided. These will be available during the recording for people to review later. That’s great.
I’ve got a question if that’s alright. Firstly, I want to thank the speakers for their insightful information. There were many common themes across all presentations. A frequently raised question when discussing with industry professionals concerns the use of portable air cleaners and in-room UVGI in its various forms. Do you anticipate challenges with ongoing maintenance, mobility, and testing of these portable devices that might impact their long-term performance? And consequently, their effectiveness in controlling infections in the built environment.
Jon Douglas 1:23:22
I’ll address that question. Yes, maintenance and the potential for portable devices to be turned off present concerns. We’ve observed this issue in practice. There’s a distinction between portable devices and in-room air cleaning systems. In-room filtration devices, which can be integrated into the ceiling and automated, offer a more permanent solution and are likely to have a longer lifespan than portable units that can easily be unplugged or moved.
Donald Weekes 1:23:59
Okay, thank you, Bill. This question is specifically for you. Has the calculator been made public at this point?
William Bahnfleth 1:24:07
The calculator that was used to develop Standard 241 has not been made public, as it wasn’t developed in a form suitable for distribution. However, the committee recently voted to develop something that could be distributed in the future. A technical and journal paper, led by Ben Jones from Nottingham University in the UK, is being written to outline the methodology. We hope it will be published soon, pending peer review. I hope we will eventually have something shareable, as a good partnership with public health authorities requires them to decide on the risk parameters that are appropriate for their specific contexts.
Donald Weekes 1:25:03
This raises a question related to the concerns many have expressed in the Q&A about the role of public health agencies. Who is responsible for determining when there’s a need to shut down or close facilities? How do we bridge the gap between the engineering community represented here and public health authorities who might be listening or will hear about our discussions? How do we involve them and help them understand the work of the engineering group?
Erik Malstrom 1:25:49
I’ll address this, keeping specific details anonymous. We’re currently navigating this challenge of aligning public health agencies with those responsible for buildings, from standards setting to design and operation. This situation ranges from being a challenge to potentially confrontational. On the building side, there’s often a reflexive resistance to measures perceived to incur additional costs, energy use, or extra work, coupled with a desire to move past the pandemic. Public health agencies typically find themselves struggling in these discussions. The success of integrating stronger public health requirements into building practices hinges on political will and concerted effort. It’s important to note that changes will likely be implemented unevenly due to the localized governance of building codes and standards. While I’m cautiously optimistic about progress, it will require significant effort and advocacy from those committed to this cause.
Brett Cole 1:27:43
Another question comes from Anna, highlighting the energy and material savings achieved through adaptive reuse of buildings rather than new constructions. New building regulations are beneficial but can be challenging or inconsistently applied to existing buildings. Could any panel member discuss the adaptation of these changes in the context of new builds versus existing buildings?
Patrick Chambers 1:28:14
From my experience, there’s a significant demand for retrofitting, especially in healthcare facilities, to enhance outdoor air rates or filtration levels. However, the constraints of existing infrastructure often make it challenging. For instance, merely upgrading filtration efficiency can necessitate larger fans and increased power, leading to additional costs and sometimes impracticalities.
William Bahnfleth 1:28:52
The approach depends on the compromises we’re willing to accept, especially during emergencies. For example, plugging an air cleaner into an existing outlet allows work continuity instead of home quarantine, representing a viable compromise. Furthermore, upper room UV can be implemented in existing spaces with minimal power impact. The situation calls for the professional and facilities management communities’ creativity to evaluate their buildings and devise suitable solutions, understanding that there won’t be a universal solution for all scenarios.
Donald Weekes 1:29:34
Regarding small handheld and desktop air purifiers, what does the panel think about their efficacy? Are they creating clean air for an individual, or do they have a broader impact? Have any of you encountered them in your field operations or research?
Erik Malstrom 1:30:07
Our data shows that when these units are properly sized and positioned within rooms, they can be very effective. However, the sustainability of using such devices is questionable. For instance, schools making bulk purchases of these air cleaners face challenges with maintenance and filter replacement costs. Moreover, their placement can be altered by individuals, reducing their effectiveness. Thus, while they may serve as a temporary solution in emergencies, central management and design of air purification are preferable for long-term efficacy.
William Bahnfleth 1:31:18
My personal experience with portable HEPA filter units during last summer’s wildfire smoke event validated their effectiveness. By increasing the fan speed of the units, I significantly reduced indoor PM2.5 levels despite high outdoor air quality index values. This experience underscores the potential of such devices, though we often rely on assumptions about their performance without direct knowledge.
Patrick Chambers 1:32:16
In hospitals, the widespread use of portable air purifiers as a quick fix has led to safety issues and maintenance challenges, including the lack of mandatory testing procedures applied to these devices. However, the industry’s creativity can lead to innovative solutions, such as reticulated suction systems, which could effectively capture and exhaust air without the drawbacks associated with portable units.
William Bahnfleth 1:33:13
The problems you’re discussing revert to the lack of a plan when this started. It was a panic mode response. I know of major medical centers in the US where they knocked holes in walls and installed new 100% outside air handling units to force in a lot of outside air, which didn’t work very well either.
Donald Weekes 1:33:37
Many attempts during the pandemic didn’t work well. Linsey Marr raised a question about personal portable CO2 monitors and their use and interpretation of data by non-technically trained individuals. Any thoughts?
Jon Douglas 1:34:05
Firstly, CO2 is a measure of the amount of outside air per person. While they are useful tools, they are not a complete indicator of indoor air quality. For example, CO2 levels on airplanes can be about 2000 ppm, suggesting poor air quality, but in reality, there’s significant filtration happening that CO2 sensors cannot detect. So, it’s a good tool, but not the whole story.
William Bahnfleth 1:34:39
Relying on CO2 levels as design criteria ignores the benefits of other controls like filtration and UV. Recent recommendations for very low CO2 concentrations disregard the potential of these technologies and focus heavily on outdoor air, which is energy-costly.
Patrick Chambers 1:35:19
I had a discussion with a water quality specialist who described the dilution strategy as cheating. I think about how we might maintain air quality in a Mars habitat, where there’s no benefit of dilution. On the International Space Station, for example, they have to be very specific about targeting pollutants since there’s no outside air for dilution.
Donald Weekes 1:36:42
Thank you to all the speakers, my co-moderator, and the attendees. There will be a fourth session in this series of lessons learned coming up shortly.
Brett Cole 1:37:07
Thanks, everybody. Appreciate it.
Watch the other sessions of the 6-part IAQ CLEAN Lessons Learned series
Navigating the H5N1 Challenge
Go to this sessionThe Critical Role of IAQ in Infection Prevention
Go to this sessionBridging the Gap Between Current IAQ Assessments and Evolving Biosensing Technologies in Built Environments
Go to this sessionUnraveling Infectious Disease Transmission in the Built Environment
Go to this sessionIndoor Air Quality as a Public Health Strategy to Reduce the Risk of Infectious Disease Transmission in the Built Environment
Go to this sessionSponsor Spotlight

Johnson Controls
At Johnson Controls (NYSE:JCI), we transform the environments where people live, work, learn and play. As the global leader in smart, healthy and sustainable buildings, our mission is to reimagine the performance of buildings to serve people, places and the planet. Building on a proud history of nearly 140 years of innovation, we deliver the blueprint of the future for industries such as healthcare, schools, data centers, airports, stadiums, manufacturing and beyond through OpenBlue, our comprehensive digital offering. Today, with a global team of 100,000 experts in more than 150 countries, Johnson Controls offers the world’s largest portfolio of building technology and software as well as service solutions from some of the most trusted names in the industry. Visit www.johnsoncontrols.com for more information and follow @Johnson Controls on social platforms.

American Industrial Hygiene Association (AIHA)
AIHA is the association for scientists and professionals committed to preserving and ensuring occupational and environmental health and safety (OEHS) in the workplace and community. Founded in 1939, we support our members with our expertise, networks, comprehensive education programs, and other products and services that help them maintain the highest professional and competency standards. More than half of AIHA’s nearly 8,500 members are Certified Industrial Hygienists, and many hold other professional designations. AIHA serves as a resource for those employed across the public and private sectors and the communities in which they work.
Have a question about the event?
Connect with IBEC experts directly! Drop your queries below, and let's further the dialogue on preventing the spread of infectious diseases.