CLEAN Lessons Learned
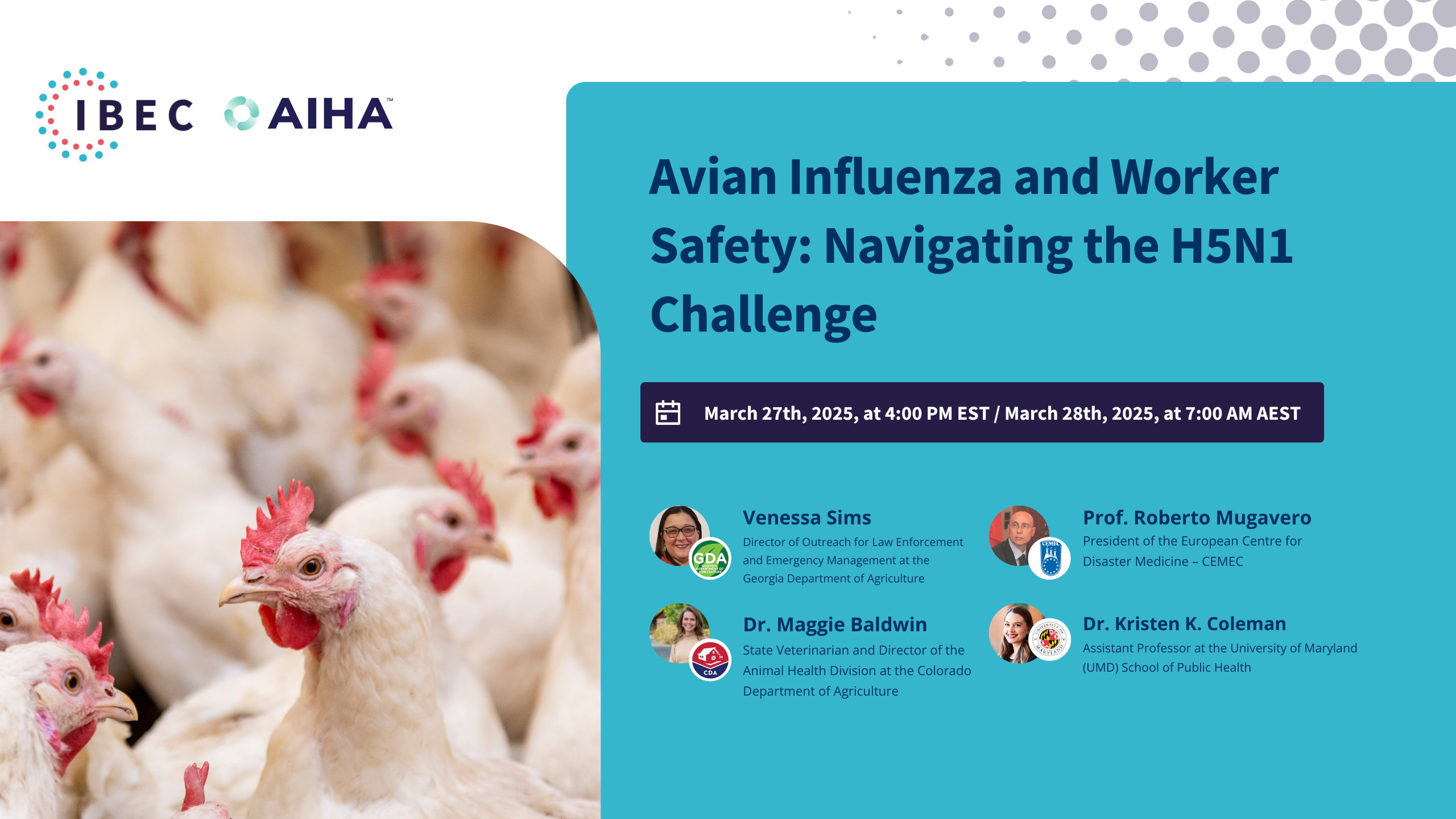
Avian Influenza and Worker Safety:
Navigating the H5N1 Challenge
In the sixth installment of our six-part CLEAN Lessons Learned series dedicated to worker safety and infectious disease preparedness, we spotlighted the critical risks posed by H5N1 avian influenza and its impact on occupational health.
We analyzed the occupational hazards of H5N1 for frontline workers, including poultry workers, veterinarians, and wildlife handlers. By delving into biosecurity measures, mental health considerations, and outbreak response strategies, we aim to comprehensively understand how organizations and policymakers can mitigate risks and enhance workforce protection.
Watch the recording or read the transcription to explore how safety measures can protect workers in high-risk environments and how surveillance, ventilation, and health protocols can be leveraged to prevent outbreaks and minimize impact. The panel featured distinguished experts from the European Center for Disease Medicine (CEMEC), the Georgia Department of Agriculture, the University of Maryland and the Colorado Department of Agriculture. These panelists brought a wealth of knowledge in infectious disease management, public health, and occupational safety. Their insights will be invaluable in guiding our discussions and strategies toward a safer, more prepared workforce.
- One Health Approach Is Essential: A coordinated response across animal health, public health, environmental health, and industry is critical to effectively managing and preventing zoonotic disease outbreaks like H5N1.
- Worker Safety Must Be a Priority: Protecting agricultural and animal health workers—including veterinarians, poultry handlers, and dairy staff—is fundamental. PPE access, fit-testing, training, and mental health support are vital to response plans.
- Felines Are Emerging as a High-Risk Species: Dr. Kristen Coleman’s research highlights domestic cats as particularly vulnerable to H5N1. With a case fatality rate of over 70% among PCR-confirmed cases, this underscoring the importance of surveillance in companion animals.
- Cross-Border Collaboration Is Crucial: Professor Roberto Mugavero emphasized the need for enhanced cooperation across European countries, particularly for surveillance, early warning systems, and harmonized outbreak responses.
- Colorado’s Dairy and Poultry Sectors Were Heavily Affected: Dr. Maggie Baldwin shared that 75% of Colorado dairies and millions of poultry were impacted, requiring coordinated quarantine, behavioral health support, and unique response strategies for each sector.
- Air Sampling Shows Promise but Faces Barriers: Though bioaerosol sampling has demonstrated the presence of airborne pathogens, broader implementation remains limited by logistical, financial, and public health concerns.
- Biosecurity Must Be Comprehensive and Adaptive: Even facilities with robust protocols have experienced repeat infections, suggesting that traditional biosecurity needs to evolve—possibly including technologies like HEPA filtration in poultry operations.
- Public Communication and Industry Trust Are Game-Changers: Transparent, unified messaging across state agencies and strong collaboration with industry partners helped build public confidence and compliance during the outbreak.
- Zoonotic Spillover Remains a Persistent Global Risk: Experts agreed that sustained transmission of avian influenza among mammals is a novel and concerning trend—one that requires ongoing research and preparedness.
- Coordination Is Not Enough Without Cooperation: As Professor Mugavero noted, true progress requires more than structural coordination—it depends on the willingness of diverse stakeholders to collaborate proactively and consistently.

Venessa Sims
Director of Outreach for Law Enforcement and Emergency Management at the Georgia Department of Agriculture
Venessa A. Sims, MEP, GA-CEM, is the Director of Outreach for Law Enforcement and Emergency Management at the Georgia Department of Agriculture. She serves as a liaison and supports education and outreach for the food and agriculture sector’s emergency management, law enforcement, and homeland security duties.
Venessa is the Georgia representative for the Southern Animal and Agriculture Disaster Response Alliance (SAADRA) and served as the Past Board President and a current Board Member for the National Alliance of State Animal and Agriculture Emergency Programs (NASAAEP) and the Heritage Emergency Response Alliance (HERA).
Venessa is the Emergency Support Function (ESF) 11 Coordinator for the state of Georgia and coordinates response activities at the State Operations Center (SOC) for ESF 11 during activations, chairs ESF 11 planning, coordination, and exercise support activities, and coordinates ESF 11 recovery endeavors. She is the Training & Exercise Coordinator for the Department, where she works collaboratively with local, state, federal, and private sector partners to plan, train, and implement exercises related to food and agriculture and public health.
She was the VISTA FORGE-ATL FSE Unified Commander (UC) and chaired the Planning Committee for animal decontamination operations. She routinely serves as a subject matter expert for nationwide animal decontamination training and exercises. She served as the Food Defense UC for Super Bowl LIII and 2025 College Football in Atlanta. As a state representative, she has served on the AVMA CDEI Committee and the FDA FSMA Intentional Adulteration Workgroup.

Prof. Roberto Mugavero
President of the European Centre for Disaster Medicine – CEMEC
Prof. Roberto Mugavero is the President of the European Centre for Disaster Medicine – CEMEC – a specialized centre of the Council of Europe’s EUR-OPA Agreement. With a degree in Environmental Engineering, he is also the Director and a Professor at the CUFS – Center for Security Studies at the University of San Marino Republic. He holds prominent roles at multiple institutions, including the University of Rome “Tor Vergata,” the University of Rome “Sapienza,” and the University of Padua in Italy; the NATO School in Oberammergau, Germany; and the NATO JCBRN CoE in Vyskov, Czech Republic. Prof. Mugavero oversees numerous master’s and advanced programs, specializing in international security studies, environmental and CBRNe risk management. As a renowned expert in security and defense, he chairs the Italian research institute “Observatory on Security and CBRNe Defence – OSDIFE.” Additionally, he significantly impacts global discourse through his lectures, publications, and leadership at various conferences. Beyond academia, Prof. Mugavero is deeply involved as a volunteer Officer in the Italian National Fire and Rescue Service at the Ministry of Interior and actively engages in EU and international security and defense research programs. His commitment is further demonstrated through direct participation in emergency activities and exercises.

Dr. Kristen K. Coleman
Assistant Professor at the University of Maryland (UMD) School of Public Health
Dr. Kristen K. Coleman is an Assistant Professor at the University of Maryland (UMD) School of Public Health and an Affiliate Assistant Professor at the UMD Department of Veterinary Medicine. Dr. Coleman is a former Senior Research Fellow in the Emerging Infectious Diseases Programme at Duke-NUS Medical School and the Department of Medicine at NUS Yong Loo Lin School of Medicine in Singapore. She earned her BA in Global Studies from the University of Toledo (UT) and her PhD in Biology (Ecology and Organismal Biology) from the Department of Environmental Sciences at UT. Her research focuses on the environmental detection, epidemiological surveillance, and transmission of emerging and zoonotic pathogens – primarily respiratory viruses such as influenza virus, adenovirus, and coronavirus. She leads the bioaerosols research team within the Public Health Aerobiology Laboratory (PHAB Lab) and has authored several key research papers on airborne transmission of SARS-CoV-2. She is the first UMCP faculty member to be selected as a University of Maryland Baltimore (UMB) Institute for Clinical & Translational Research (ICTR) KL2 Clinical Research Scholar.
Dr. Coleman champions a One Health approach to understanding pandemic respiratory virus transmission and has engaged in One Health infectious disease research in Singapore, Malaysia, Vietnam, and China. She is a former member of the Duke One Health Research team at the Duke Global Health Institute and is now a U.S.-based collaborator of the University of Texas Medical Branch (UTMB) One Health Task Force. Dr. Coleman is currently conducting research on avian influenza virus in felines and the spillover risk to small animal veterinarians and animal shelter workers.

Dr. Maggie Baldwin
State Veterinarian and Director of the Animal Health Division
Dr. Maggie Baldwin joined the Colorado Department of Agriculture in January 2017, serving in several roles before being appointed as the Colorado State Veterinarian in May 2021. In this position she manages CDA’s Animal Health Division through planning, directing and executing all programs, policies and cooperative agreements with other governmental agencies.
Dr. Baldwin earned her DVM from the University of Minnesota’s College of Veterinary Medicine in St. Paul. She began her career in public service as a Supervisory Public Health Veterinarian with USDA Food Safety and Inspection Service and also served as a Veterinary Medical Officer with USDA Animal and Plant Health Inspection Service.
Ken Martinez 00:00
Good afternoon to everyone in the United States, good evening to those in Europe, and good morning to those in Australia who may be joining us. Welcome to this live webinar session hosted by the Integrated Bioscience and the Built Environment Consortium (IBEC) and the American Industrial Hygiene Association (AIHA), focusing on Avian Influenza (H5N1) and Worker Safety: Navigating the H5N1 Challenge.
My name is Ken Martinez. I am the current President of IBEC. I’m an environmental engineer and a certified industrial hygienist with over 40 years of experience in the field of biosecurity and infection prevention.
IBEC is made up of many dedicated members, including 30 members who serve on our Science Advisory Board (SAB). These members span across the United States, Europe, Australia, and the Asia-Pacific region. Our SAB is overseen by our Chief Science Officer, Dr. Stéphane Bilodeau.
Our mission at IBEC is to bring science into real-world application and to reinforce the understanding that buildings, pathogens, and people must work together to reduce the risk of airborne infectious disease.
This brings us to today’s CLEAN Lessons Learned series on pathogens and buildings. In this session, however, we expand our focus to include a fourth factor—other species, particularly domesticated animals. We’ll be discussing how a virus impacting poultry has not only decimated egg and food supplies, but also led to human cases of a serious, life-threatening respiratory infection.
This session is generously sponsored by the American Industrial Hygiene Association (AIHA), and is made possible thanks to the excellent technical support provided by the team at Firebrand Creative. Thank you, Firebrand.
A warm welcome to all of you, and to our fellow members at AIHA. We’d also like to thank the team of volunteers who keep IBEC running and have made it possible for us to be with you today to share knowledge and gain a deeper understanding of this key pathogen.
Today, we’re bringing together diverse expertise and perspectives on the risks of avian influenza and how to prevent and control it. We’ll be exploring the illness and its progression to date, and looking at the resources needed to respond to an outbreak of this significant zoonotic disease—one that is currently spreading not just in the United States, but also in countries where our international colleagues are located.
We’ll discuss how to identify and detect the virus, how to share information, and—above all—how to stay safe when entering indoor spaces with non-human occupants, including farm animals, who are at risk of becoming infected.
Our speakers and moderators have developed thoughtful questions to guide today’s discussion. We’ll begin by presenting those, and we encourage you to submit your own questions using the Q&A box located on the right side of your screen.
If we’re unable to address your question during the session, we’ll do our best to share it with the panelists afterward. Please be sure to include your name and direct your question to a specific speaker if applicable.
This session is scheduled to last for 90 minutes. If you experience any technical issues or have questions about the session’s format, feel free to leave a comment.
At the end of the session, we’ll give a brief update on IBEC’s latest work and share how you can stay engaged with us moving forward.
Now, I’d like to introduce my co-moderator, Venessa Sims. Ms. Sims has worked with the Georgia Department of Agriculture for 25 years and currently serves as the Director of Outreach for Law Enforcement and Emergency Management. She is also engaged as the Emergency Support Function 11 Coordinator for the Georgia Emergency Management and Homeland Security Agency.
Venessa, given your lifetime involvement in food defense and emergency management, I’ll turn it over to you now to introduce yourself and our panelists. But I believe you have a poll you’d like to run first—go ahead.
Venessa Sims 04:03
Greetings, everyone. I’m Venessa Sims, and I’ve had the distinct pleasure of graduating from Davidson College. I’ve worked in animal and agricultural emergency management since Hurricane Katrina and have had the opportunity to collaborate with our local, state, and federal partners throughout that time.
I’ve worked across various departments and currently serve as a liaison in my role. I also train and partner in the National Incident Management System (NIMS) and Incident Command System. I’ve served as an Incident Commander for food defense during the Super Bowl and led animal decontamination efforts for events like Vista Forge in Atlanta. My work also includes planning, response, and recovery for natural disasters in the state of Georgia.
Additionally, I serve on the Southern Animal Agriculture Disaster Response Alliance (SAADRA) and the National Alliance of State Animal and Agricultural Emergency Programs (NASAAEP).
As Ken mentioned, we are so grateful to have you all here today. I’d like to start by directing your attention to a few quick polls. We’d like to learn more about your background and knowledge regarding highly pathogenic avian influenza (HPAI), as well as biosecurity.
If you look at the bottom of your screen, the first question asks whether or not you’ve ever been involved in a HPAI incident response. Please take a moment to respond “yes” or “no.”
The next question asks about your role in an HPAI response. Are you regulatory? A support agency partner? Do you work in a lab, in industry, or fall under “other”? With such a diverse and international audience—participants from the U.S., Europe, and Australia—we’d love to better understand who’s joining us today.
The final question is about your current knowledge of available biosecurity resources. Your options are: no knowledge, limited knowledge, or extremely knowledgeable.
Again, please take a moment to respond. We have an amazing slate of speakers today, and we hope you walk away with increased knowledge across all of these areas.
Without further ado, I’d like to introduce our panelists—starting with Professor Roberto Mugavero, who is the President of the European Center for Disaster Medicine. He holds a degree in Environmental Engineering and is the Director and a professor at the CUFS Center for Security Studies at the University of San Marino in the Republic of San Marino.
He also holds prominent roles at multiple institutions, including the University of Rome Tor Vergata, the University of Rome Sapienza, and the University of Padua in Italy. In addition, he’s affiliated with the NATO School in Oberammergau, Germany, and the NATO Joint CBRN Centre of Excellence in the Czech Republic.
Professor Mugavero oversees numerous master’s and advanced programs specializing in international security studies and CBRN risk management. He is a renowned expert in security and defense, and chairs the Italian Research Institute Observatory on Security and CBRN Defense. He is also deeply involved in EU and international security and defense research programs, and volunteers as an officer with the Italian National Fire and Rescue Service at the Ministry of Interior. His commitment is demonstrated through both his academic leadership and his direct participation in emergency activities and exercises.
Next, we have Dr. Kristen Kelli Coleman, Assistant Professor at the University of Maryland School of Public Health. Dr. Coleman is a former senior research fellow in the Emerging Infectious Diseases Program at Duke-NUS Medical School and the Department of Medicine at the Yong Loo Lin School of Medicine in Singapore.
She earned her B.A. in Global Studies from the University of Toledo and her Ph.D. in Biology, Ecology, and Organismal Biology from the Department of Environmental Sciences at UT. Her research focuses on environmental detection and epidemiological surveillance of emerging and zoonotic pathogens—primarily respiratory viruses such as influenza virus, adenovirus, and coronavirus.
She leads the Bioaerosols Research Team with the Public Health Aerobiology Laboratory and has authored several key studies on the airborne transmission of SARS-CoV-2. She is also the first University of Maryland College Park faculty member to be selected for the University of Maryland Baltimore Institute for Clinical and Translational Research—congratulations to her on that.
Dr. Coleman champions a One Health approach to understanding the transmission of pandemic respiratory viruses and has conducted research in Singapore, Malaysia, Vietnam, and China. She was previously part of the Duke One Health Research Team at the Duke Global Health Institute and is currently a U.S.-based collaborator with the University of Texas Medical Branch One Health Task Force.
Dr. Coleman is currently conducting research on avian influenza virus in felines and the spillover risk to small animal veterinarians and animal shelter workers.
Our final speaker is Dr. Maggie Baldwin, who serves as the State Veterinarian and Director of the Animal Health Division at the Colorado Department of Agriculture.
Dr. Baldwin joined the Colorado Department of Agriculture in January 2017, serving in several roles before being appointed as State Veterinarian in May 2021. In her current role, she manages the department’s Animal Health Division, planning, directing, and executing all programs, policies, and cooperative agreements with other government agencies.
She earned her Doctor of Veterinary Medicine from the University of Minnesota College of Veterinary Medicine in St. Paul. She began her public service career as a Supervisory Public Health Veterinarian with the USDA Food Safety and Inspection Service and later served as a Veterinary Medical Officer with the USDA Animal and Plant Health Inspection Service
At this time, I’d like to invite each of our panelists to say a quick hello and share what they hope to gain or contribute through today’s discussion.
Dr. Baldwin, would you mind unmuting and kicking us off?
Maggie Baldwin 13:04
Okay, how’s that? Can you hear me? Great—thank you. Fantastic.
Thank you very much, Venessa and Ken. Good to see both of you this afternoon. I just finished another two-hour session on HPAI with a different group, so I’m happy to jump right back into it.
Is this the time you’d like me to share my screen and slides, or just say hello?
Venessa Sims 13:28
Yes, if you could just share a brief insight on what you’d like to gain from today’s session, and then I’ll ask Dr. Mugavero and Dr. Coleman to do the same. After that, we’ll ask each of you to take about 10 minutes to discuss your role in addressing highly pathogenic avian influenza.
Maggie Baldwin 13:44
Absolutely. As the State Veterinarian in Colorado, we’ve had a lot of experience with HPAI—both on the poultry side and more recently on the dairy side. Colorado has been one of the most impacted states over the last three years, particularly with our layer poultry facilities, and now with dairy as well.
So I’m really excited to talk with all of you and with the other panelists today, and to learn more—especially around the topic of worker safety. I’m very interested to hear what others are doing in this space. I’m also happy to share what Colorado has done over the past couple of years, particularly during our dairy outbreak over the last year.
Thanks again, Venessa—I appreciate the opportunity.
Venessa Sims 14:23
Thank you, Dr. Baldwin.
Dr. Coleman, if you could say hello to everyone and share what you’d like to gain from today’s session.
Kristen Coleman 14:32
Hi, everyone. Thank you so much for inviting me. I’d really like to share what I’ve done so far in avian influenza virus research—how what I’ve learned through past studies has shaped my understanding today, and how I approach the emergence of infectious viruses like avian influenza.
I’m especially looking forward to hearing from Dr. Baldwin and other veterinarians on how they are planning to manage the situation, particularly given that the virus is now infecting mammals. As we know, there have been growing concerns about domestic cats being affected. I’m very interested in how the risks posed by companion animals—presumed to be infected with avian influenza viruses—are being handled in those cases.
That’s what I’m hoping to explore today. Thank you.
Venessa Sims 15:29
Thank you, Dr. Coleman.
Dr. Mugavero, if you could unmute, sir.
Roberto Mugavero 15:40
Great. Thank you so much. It’s my pleasure to be here with you—truly an honor to join this event.
As mentioned, I serve as Chair of the European Center for Disaster Medicine. Our focus is primarily on disasters and public health. Increasingly, our attention is turning to emerging and re-emerging diseases.
Part of our mission is understanding how to create the right environment to address diseases and public health concerns comprehensively. This includes not only response, but also—most importantly—prevention and mitigation strategies.
That’s all from me for now. Thank you.
Venessa Sims 16:46
Thank you, sir.
Now, Dr. Baldwin, we’ll circle back to you. If you could take about 10 minutes to discuss your role in addressing highly pathogenic avian influenza, we’ll then move on to Dr. Coleman, and conclude with Dr. Mugavero.
Maggie Baldwin 17:11
Yes, I’m excited to talk about Colorado’s response, give an overview, and I’m especially looking forward to the questions and discussion later. I’d like to start with a brief overview of Colorado’s industry and how it’s been impacted.
Our poultry industry includes just over 4 million laying hens, though that number has been as high as 5.5 million in the past. These birds are spread across several commercial sites that produce just under a billion table eggs annually. We also have a complex of broiler breeder facilities on the Western Slope with around 650,000 breeding birds, which produce more than 80 million fertile eggs per year that go on to become broiler chickens. Additionally, we have some niche layer flocks, specialty flocks, waterfowl, and game birds. And of course, we also have exhibition birds.
On the dairy side, Colorado has around 200,000 milking cows spread across a little over 100 dairy farms. For bulk tank testing, this breaks down to 86 individual dairy cow premises. Our producers take pride in being ranked second nationally for milk produced per cow, and 13th in total milk production, generating about 5.2 billion pounds of milk annually.
This outbreak has been the first time I, and many others, have had to manage a situation affecting both of these industries simultaneously. We’re used to balancing the needs of different sectors, but this was a unique situation—dealing with poultry and dairy, two very distinct industries affected very differently by the same virus.
On the dairy side, the virus causes illness, and we saw significant clinical signs in our herds—ranging from 10% to 30% of cows showing symptoms. In poultry, as we all know, HPAI is a high-mortality disease that can wipe out entire flocks. So the challenge became: how do we respond to a disease that affects these two sectors so differently?
Of course, we also had to consider the people involved—not just those working on the farms, but also the responders. This was one of the most robust One Health responses we’ve seen, and it required careful coordination.
Prior to my time as State Veterinarian, Colorado had a zoonosis MOU (Memorandum of Understanding) with our public health colleagues. CDA is the Colorado Department of Agriculture, and CDPHE is the Colorado Department of Public Health and Environment. This MOU, in place since 2007, outlines coordination mechanisms for zoonotic disease response. I’m pleased to share that it’s now undergoing a major revision to become an official One Health MOU, which will also include our state wildlife agency.
When it comes to HPAI in poultry, we’ve had well-established response plans for years. These include quarantining, surveillance, depopulation, disposal, and decontamination. In Colorado, we deploy a Type 3 state incident management team and set up an incident command post, typically at the local fire station. This field presence is vital—producers know who to contact and feel supported.
We also work closely with CDPHE on public health, including on-site monitoring. Notably, this past year was the first time we provided behavioral health support on-site during every operational period. That support extended not just to responders, but also to poultry producers and their workers.
On the dairy side, we had to build the response from scratch. While HPAI was already a reportable disease in Colorado, it hadn’t previously been species-specific. One major step we took was assigning each affected dairy a case manager—either a veterinarian from my team or someone from USDA or another state. This gave each producer a single point of contact.
We quarantined affected dairies, specifically the lactating cows, and required them to complete an epidemiological questionnaire. Biosecurity became a condition of quarantine. These visits were coordinated with public health officials, so they could conduct joint site assessments. That coordination was well received—producers appreciated a unified visit rather than multiple, separate ones. CDPHE also distributed PPE during these visits.
Now, briefly, some numbers. Prior to B3.13—the virus strain involved in the recent spillover—we had 37 poultry facilities affected, involving over 6.3 million domestic poultry. You might notice that number is higher than the number of birds in the state—that’s because some facilities were hit multiple times.
Following the emergence of B3.13 in July of last year, we saw 64 of the 86 dairies (roughly 75%) affected, along with 3.3 million poultry. Spillover also occurred in domestic cats, and we had confirmed human cases and even infections in captive big cats.
This has been a truly unique response. In avian influenza outbreaks, we must balance multiple priorities: animal health and welfare, human health and safety, and virus burden in the environment. These are interdependent—focusing too much on one can jeopardize the others. For example, if we focus only on human safety, we might compromise animal welfare or allow more virus in the environment.
To address this, we worked with the Governor’s Office and CDPHE to develop a plan that ensured checks and balances. On the human health side, this included additional screening, testing, isolation protocols, and prophylaxis when needed. We also emphasized PPE—not just distribution, but proper use and compliance.
This was a real challenge. The response occurred during summer, and the heat made compliance with full PPE difficult, especially in dairy and poultry environments.
We also considered alternatives to standard depopulation practices, exploring less labor-intensive methods. For example, we used CO₂ carts, even at large layer facilities, but these are extremely time- and labor-intensive.
Lastly, when I talk about worker safety, I also include my team—state responders and USDA partners. In Colorado, we emphasize taking care of our people. That includes behavioral health support, communication systems (like Starlink and radio setups), and yes—even snacks. Keeping people fed and supported helps ensure an effective and compassionate response.
With that, I’ll stop sharing my screen. Venessa, I’ll turn it back over to you for the next speaker. Thank you.
Venessa Sims 27:50
Thank you, Dr. Baldwin—very, very engaging.
Now I’d like to turn it over to Dr. Coleman. If you could share your role in the highly pathogenic avian influenza (HPAI) response.
Kristen Coleman 28:23
Can you all see my screen?
Venessa Sims 29:09
Okay, I think we might be able to hear you now. Are you good? Can you hear me?
Kristen Coleman 29:14
Yes, I can hear you.
Venessa Sims 29:23
Okay, everyone—we’re experiencing a few technical difficulties, so we’ll pause for just a moment to see if Dr. Coleman can rejoin us.
Let’s give it a second, and if not, we’ll go ahead and invite Dr. Mugavero to share his remarks, and then we’ll circle back to Dr. Coleman.
Roberto Mugavero 29:57
I’m here’m here—great. I’m not sharing any slides, but I’d like to offer a few reflections on the European context and the current efforts underway.
Between September and December 2024, Europe reported approximately 657 detections of highly pathogenic avian influenza (HPAI) viruses in both domestic and wild birds across 27 European countries. The clusters were primarily identified in areas with high poultry density, indicating significant farm-to-farm spread of the virus. We also observed that the virus expanded its geographic and host range, leading to increased detection and mortality events, especially among gulls and crows.
On the other hand, no new virus detections in mammals were reported in Europe during this period. The overall risk of infection with the currently circulating influenza viruses remains low for the general public at the European level. However, we consider the risk to be low to moderate for individuals who are occupationally or otherwise exposed to infected animals or contaminated environments.
At our center, which focuses on public health and disaster and mass emergency events, we are especially concerned with protecting workers through safety measures—both in general for biological events and in particular for emerging infectious disease outbreaks such as this one. In this context, we have developed a set of recommendations aligned with both European and national guidelines for worker and responder protection.
These include standard recommendations such as the use of personal protective equipment (PPE)—gloves, long-sleeved coveralls, waterproof aprons, and respiratory protection. But one key lesson we’ve learned is that simply distributing PPE is not enough. In many cases, the PPE does not properly fit or meet national standards for usage. That’s why it is essential not only to supply protective equipment but also to provide comprehensive training on how to wear and use it correctly.
Basic hygiene practices must also be emphasized: handwashing after handling livestock or contaminated materials, covering cuts and abrasions with waterproof plasters, and avoiding contact with the face—mouth, eyes, and nose. These may seem like simple recommendations, but our experience shows they are frequently overlooked or improperly followed. That’s why continuous training and information sharing with both workers and responders are critical to mitigating these threats.
Biosecurity measures also play a vital role. These include preventing contact between poultry and wild birds, limiting movement around poultry enclosures, controlling access by vehicles, people, and equipment, ensuring proper disposal of manure and dead animals, and regularly cleaning and disinfecting animal housing and equipment.
Vaccination is another important and complex topic. Beyond response, prevention is key. Poultry vaccination can be an effective preventive measure. For workers at higher risk, we also recommend seasonal influenza vaccination to reduce the potential for co-infection and viral reassortment.
We are working to create the right environment for both workers and responders by providing comprehensive training on the risks associated with avian influenza and other biological threats. This includes ensuring awareness of infection symptoms and knowledge of the proper procedures for reporting suspected cases.
In summary, the strain of avian influenza circulating in Europe continues to pose challenges. The main tactical activities underway focus on ensuring proper PPE use, raising awareness, and strengthening worker training. At a more strategic level, we are emphasizing ongoing surveillance, adherence to safety protocols, and improving preparedness to protect both animal and human health.
This has been just a brief overview of what we are experiencing in Europe and the measures we are putting in place to reduce infection rates and mitigate the broader consequences of these events. Thank you.
Venessa Sims 39:05
Thank you, Professor Mugavero. I really appreciate both you and Dr. Baldwin highlighting the importance of worker safety. It’s such a key cornerstone of our entire operational response. We appreciate you sharing these insights, and I’m sure we’ll learn even more as the discussion continues.
Dr. Coleman—welcome back.
Kristen Coleman 39:30
Hello everyone—I’m back! Sorry, I was kicked off earlier. Let’s try this again. I’m going to share my screen—fingers crossed… Okay, all good? Great, thank you.
My talk today focuses on avian influenza virus research that I’ve conducted since 2017–2018, leading up to the present. I’ll share what I’ve learned about transmission and the potential zoonotic risk to animal workers. I’ll begin with a brief overview of the One Health research I’ve done, then discuss some of my current work, including a look at the history of avian influenza in felines, and finally, I’ll touch on prevention.
Since the emergence of SARS-CoV-2, we’ve all become acutely aware of the global challenge of early detection of novel virus incursions. It remains incredibly difficult to quickly identify and robustly track pandemic threats in time to launch an emergency response. We need to strengthen our biosurveillance efforts.
One approach I’ve used throughout my research career is bioaerosol sampling as a non-invasive tool to monitor for viruses like avian influenza at the human-animal interface and in occupational settings.
In 2017, I hosted my first Emerging Respiratory Virus Threats workshop with the Duke One Health team in Hanoi, Vietnam. One of the main goals was to teach veterinary partners how to use bioaerosol sampling equipment, enabling them to monitor occupational exposures in farm environments and live poultry markets.
Our first study, in partnership with Vietnamese colleagues, focused on a live poultry market in Hanoi called Ha Vy Market. It’s a massive space—about two hectares—with 200 registered shops and approximately 80,000 to 200,000 live birds sold daily. The objective was to use the sampling method I developed during my dissertation to detect H5 and H7 avian influenza viruses, especially H7N9, which at the time posed a cross-border risk from China.
In addition to bird-human interface studies, we also conducted surveillance at the pig-human interface—an important area, given the role of pigs in zoonotic influenza transmission, as we saw with the 2009 H1N1 pandemic. Using the same sampling method, we collected bioaerosol samples near pig pens to detect both human and animal respiratory viruses. These included influenza viruses, adenovirus, enterovirus, and porcine circovirus type 2 (PCV2).
In these studies, we not only sampled ambient air, but also measured personal exposure. For example, this photo shows a student named Rick, who wore the sampling device to measure aerosol exposure while working in the field.
Our results showed clear occupational exposure risk. We detected aerosolized human and animal viruses in these environments. In the Malaysia study, we even found PCV2 in nasal washes of animal workers. While this doesn’t indicate infection, it does confirm inhalation exposure. This highlights the risk: if it had been a novel influenza strain—or another novel coronavirus—the implications would have been much more serious.
Now, shifting to the United States: avian influenza is increasingly infecting mammals. I’ve become especially focused on felines. We’re currently in what I’d describe as a panzootic, especially with the emergence of H5N1 clade 2.3.4.4b, which has accelerated mammalian infections and transmission.
To better understand this, my PhD student and I conducted a systematic review of avian influenza infections in felines over the past two decades. The first feline case we found in the literature occurred in 2003 during a large outbreak among captive tigers in Thailand. That sparked my student’s interest, and this has since become the focus of his dissertation.
Interestingly, many domestic cat infections reported by USDA are not documented in the scientific literature. There are major gaps in our knowledge—how these cats are infected, how the virus is transmitted, and what the potential risks to humans are. These gaps matter because domestic cats are very common companion animals.
We uploaded our review to medRxiv (it’s now under peer review). We identified 607 avian influenza virus infections in felines across 18 countries and 12 species. Among the PCR-confirmed cases, the overall case fatality rate was 71.3%. For infections caused by clade 2.3.4.4b—the one currently circulating in U.S. dairy cattle and birds—the case fatality rate was 90%.
We’re not sure why it’s so high; it could be due to more severe cases being more likely to be reported, or improved surveillance. But it raises concern.
You can see from our data that reports of feline infections spiked in 2023 and continued into 2024. Our analysis doesn’t yet include a 2025 CDC report describing two households where dairy farm workers may have passed the virus to their cats—or vice versa. That will be included in our next update.
We also looked at how transmission occurs. The most common route is bird-to-cat through ingestion. This includes cats eating infected wild birds or raw poultry products. In fact, cats in South Korea and Poland recently died after eating raw chicken feet contaminated with H5N1, and in the 2003 tiger outbreak, zookeepers had fed the animals raw chicken carcasses.
A newer concern is cat infections through contaminated raw milk or colostrum from infected dairy cattle. The first such case in the U.S. was reported in July 2024, involving two domestic farm cats in Texas.
Some reported cases have unknown transmission routes, which raises additional questions: Could it be from house mice? From owners? Dr. Baldwin may be familiar with recent reports from the Colorado Health Department of two indoor-only cats with no known exposure to infected animals—cases that leave us wondering if there are transmission routes we haven’t yet identified.
Feline-to-feline transmission also occurs. It has been shown experimentally and documented in real-world outbreaks. One occurred in a New York animal shelter in 2016 involving H7N2. Though the exact number of infected cats wasn’t published, informal reports say up to 500 cats may have been involved. Another outbreak in South Korea was initially thought to be cat-to-cat but may have been caused by contaminated food.
As for feline-to-human transmission: this is the big question. We don’t have a confirmed case of a cat infecting a human, but there have been strong signals. In the 2003 Thai tiger outbreak, two humans showed evidence of seroconversion. In the New York animal shelter outbreak, both a visiting veterinarian and a shelter worker were exposed while handling infected cats.
NIOSH conducted an investigation at the New York facility and found culture-positive air and surface samples—suggesting airborne transmission is possible. This is critical to consider if we start seeing infected cats entering shelters and vet clinics in large numbers.
So how do we prevent it?
This is my foster cat, Blaze—he wants to know how to stay safe. Here are four recommendations for the general public:
Do not touch or allow pets to touch sick or dead animals or animal droppings.
Do not consume or feed pets raw meat or raw milk.
Keep a close watch on free-roaming outdoor pets. I know it’s hard—I grew up with a cat named Zero who would disappear for hours—but it’s important.
Report any respiratory or neurological symptoms in your pet to a veterinarian immediately. Cats often serve as sentinels for nearby outbreaks.
Right now, we’re doing follow-up research, including a serosurvey of domestic cats to understand how widespread the virus is in that population. We’re working with shelters, rescues, and animal welfare groups—and eventually, we hope to monitor avian influenza exposure among the animals, workers, and environments of those facilities.
If you’re interested in collaborating, feel free to reach out. I’m at the University of Maryland, and we’d be happy to work with you.
Thank you.
Venessa Sims 59:14
That was really great information. As I mentioned earlier, I serve on the Southern Animal and Agriculture Disaster Response Alliance (SAADRA) as well as NASAAEP, and we would be happy to share your work with our distribution lists to support your studies.
Now we’re going to transition. I think each of your opening remarks flowed nicely into our next question: helping us understand the professional and scientific perspectives on the current risks we face to health and food security.
Before we begin, I just want to thank you again, Dr. Coleman, for sharing those four prevention tips—they’ll be excellent for public outreach.
Dr. Baldwin, we’ll start with you. What would you like to share about the risks we’re seeing around health and food security, especially since it’s something we’re hearing about so much in the news and on social media?
Maggie Baldwin 1:00:28
Yes, thank you. That’s such an interesting question, and honestly, depending on when you ask me, I might have a different answer.
Right now, over the past four weeks or so, we’ve seen a slight decline in HPAI cases. But if I take a step back and look at our response over the last three years—especially on the poultry side—I’d say we’ve been very successful here in Colorado.
Our producers have been incredibly proactive about biosecurity. They’ve been really engaged, even before we had our first case. We held planning meetings with each of our commercial facilities and walked them through what would happen in the event of an HPAI detection. And eventually, we had to put those plans into action.
We’ve been challenged in many ways, but I think everyone has risen to the challenge. That said, in the last 12 months, we’ve encountered something we’ve never faced before—H5N1 being sustained in a mammalian population. That’s unprecedented. It’s a very different kind of risk that affects both poultry facilities and dairy operations.
On the dairy side, we definitely saw a drop in milk production at some of our plants here in Colorado. But I think this situation is pushing us to consider how we might adjust our response strategies moving forward.
I’m especially excited that we’re now exploring vaccination as an option. In Colorado, we’ve been asking for it for years. We’re not a major poultry export state, so I think we’d make a great pilot state for it. There are steps we can take to better protect our food supply and ensure business continuity.
We’re fortunate that, on the dairy side, the virus is entirely inactivated by pasteurization—which, by the way, just turned 101 years old this year. That’s why we pasteurize! So we’re confident that we can continue producing safe dairy products.
On the poultry side, we’ve already made modifications to our response protocols. For example, we now allow eggs produced more than 48 hours before the onset of clinical signs to be processed for human consumption. That change allows us to recover some of the protein value from those flocks.
So yes, there are more improvements we can make, and I think we’re heading in the right direction. We’ve already seen progress in how we respond, and I’m hopeful that continued innovation—especially in prevention—will help us strengthen our food systems even more.
Venessa Sims 1:03:26
Thank you, Dr. Baldwin. I think each of you would agree that this One Health approach has really helped guide the response.
Dr. Coleman, is there anything else you’d like to add? And then we’ll go to Professor Mugavero.
Kristen Coleman 1:03:46
I don’t have much else to add beyond what I’ve already shared, but I want to echo Dr. Baldwin’s remarks. This is absolutely a One Health issue. We’re dealing with something new—this virus is transmitting from mammals to mammals, and it’s not slowing down. So it’s likely something we’ll be grappling with for quite some time.
Venessa Sims 1:04:22
Thank you. Roberto, anything to add? You’ll need to unmute.
Okay, while we’re waiting—can each of you share any additional insights regarding the public and industry partners? How has the current avian influenza outbreak affected public perception and your engagement with key stakeholders?
I know from my role at the Department of Agriculture, we receive a lot of inquiries on the communications side, so I’d love to hear how that’s shaped your overall response—especially with industry involvement and outreach.
Maggie Baldwin 1:05:22
I’d be happy to jump in first, if that’s all right. Maybe we can go in the same order as before.
Here in Colorado, I feel very fortunate that we have strong partnerships with our industry stakeholders. One of the most important things, in my opinion, is that everyone—regardless of which agency they represent—shares a consistent message. Whether someone speaks to me, our state public health veterinarian, or our state wildlife veterinarian, they’re going to get the same answer.
Having that unified voice builds consumer confidence and public trust in how we’re managing the response.
One thing we did very effectively was hold a series of public webinars. At first, some of our public health colleagues were hesitant—they weren’t used to being in such public-facing roles. But I really believe in being transparent with our stakeholders. If they have hard questions, I want to be the one to answer them.
That openness helped build a lot of trust with the community. I wasn’t afraid to get in front of people, explain what we were doing, and talk honestly about the response. And I think the more transparent we were, the more trust we earned.
We also included our industry partners at every step—both on the dairy and poultry sides. From the very beginning, they were at the table with us. We collaborated with them as we developed our plans. We didn’t issue new orders without discussing them first. That partnership is critical—we simply can’t respond effectively without their involvement.
So I’d say we’ve been very fortunate. We had shared messaging, a unified voice, strong public engagement, and true collaboration with our industry partners. It made all the difference.
Venessa Sims 1:07:15
Thank you, Dr. Baldwin. Dr. Coleman?
Kristen Coleman 1:07:20
I don’t have anything additional to add. I primarily conduct research, so I don’t work directly with industry. That said, I do agree that it’s important to consider industrial needs. And it’s true—Americans love eggs. Talking about things like egg prices is an effective way to communicate the impact of this virus to the public because it connects to something they understand and care about.
So yes, I think we need public and stakeholder buy-in. It’s essential for helping to contain the virus. We’re doing our best from the scientific side, but we need support across the board.
Venessa Sims 1:08:08
Yes. Professor Mugavero, anything you’d like to add to what’s already been shared?
Roberto Mugavero 1:08:16
Definitely, yes. I agree. At the European level, we believe the only effective way to approach bio-emergencies and emerging diseases is through a collaborative effort—not just the business of government or responders alone. It must include the public and industries as well.
But we know that building those links, especially involving the industrial sector as true partners, can be difficult. Trust isn’t built overnight. It takes time and consistent effort. Still, it’s essential.
We need alignment—between the public, industry, government, and workers. If those groups aren’t working together, then we’re missing a critical opportunity to reduce the consequences of biological emergencies.
Venessa Sims 1:09:46
Yes, thank you. I want to echo Dr. Baldwin’s comments. Here in Georgia, our State Veterinarian, Dr. Janemarie Hennebelle, has worked closely with the Georgia Poultry Federation and the Georgia Poultry Laboratory Network. Dr. Louise Dufour-Zavala and Mike Giles at the Federation have also been key partners.
As you mentioned, it takes time, investment, and a dedicated interest to build those partnerships—whether that’s through regular calls, joint planning, or response coordination.
I also want to emphasize how far One Health has come in my own career. It’s shaped how we collaborate, how we communicate, and how we develop that “one voice, one message” approach that Dr. Baldwin spoke about.
Now, we’ll transition. Dr. Baldwin and Dr. Coleman, could you share your experiences working on a joint federal and state response to the avian influenza outbreak?
Then we’ll turn to Professor Mugavero to speak about cross-border collaboration in the EU.
Maggie Baldwin 1:11:23
Yes, I’d be happy to speak to that. As a state that has been significantly impacted over the past several years, I can say without hesitation—we absolutely could not do what we do without our federal partners. That includes USDA, CDC, FDA—all the federal agencies that have come together to support our response efforts.
While we like to think of ourselves as fairly independent, the reality is that we are also very dependent on key federal resources and collaboration.
Here in Colorado, we’ve had emergency response plans in place for quite some time. One of my favorite quotes, from Dwight D. Eisenhower, is: “Plans are worthless, but planning is everything.” It’s true—we had written plans, but what really made the difference was exercising those plans and preparing as a team. That’s what got us ready in early 2022.
We conducted tabletop exercises ahead of time, talking through coordination with USDA: how to request federal resources, how to structure our incident management team, and so on. While we always planned to use a state Type 3 Incident Management Team, we knew we couldn’t handle the response alone.
So we implemented a joint command structure. Our incident command was led jointly by myself and a USDA representative—either the Area Veterinarian in Charge or the USDA Emergency Coordinator. That meant decisions were made collaboratively and strategically.
And then, of course, my second favorite quote on planning is from Mike Tyson: “Everybody has a plan until they get punched in the mouth.” That’s exactly how it felt in 2022. We had a plan, but we really didn’t know how it would play out until the outbreak actually hit. After that, we learned quickly. Every outbreak since, we’ve known what to do. We understood the federal resource ordering system, our personnel needs, and our response structure.
We’ve built a strong partnership—and we truly couldn’t do this without our federal counterparts.
Venessa Sims 1:13:42
Very well said. Professor Mugavero, would you like to share about cross-border planning and partnerships in the EU?
Roberto Mugavero 1:13:57
Yes, thank you—and apologies, I was having some microphone issues earlier.
From a European perspective, it’s clear that the highly contagious nature of H5N1, combined with factors like interconnected trade, agriculture, and migratory patterns, demands a coordinated and united response—not just at the European level, but globally.
Cross-border collaboration is not just helpful—it’s essential.
However, even within the European Union, it can be very challenging. We are a union of countries with different health systems, veterinary networks, and regulatory frameworks. While there is guidance provided by the EU, the implementation and integration at the national level is often fragmented.
This makes collaboration even more critical—particularly for early warning and detection, rapid information sharing, laboratory results, and genomic sequencing. When we can establish the right networks and interconnections between countries, we enable faster responses before the virus crosses borders.
One key initiative I want to highlight is the Joint Surveillance Network, supported by the European Centre for Disease Prevention and Control (ECDC) and the European Food Safety Authority. This platform enables real-time information exchange. It’s a great example of how we can work together and create harmonized monitoring systems that lead to timely risk assessment and informed policy-making.
Initiatives like these also create the foundation for coordination among public health authorities, veterinary services, industry, and the public—ensuring a robust One Health approach.
Someone earlier mentioned WHO’s One Health framework, and I agree—it’s a milestone in recognizing the interconnectedness of human, animal, and environmental health. In Europe, we’re heavily invested in uniting efforts for early detection and collaborative responses. But we also recognize that this must be paired with research and innovation.
Programs like Horizon Europe (formerly FP7) are helping accelerate progress in disease control by funding research and the development of new tools, networks, and collaborative strategies.
To summarize: cross-border collaboration in the EU is absolutely necessary. We’ve made meaningful progress, but we must keep advancing—and I believe we’ll see even greater results in the near future.
Thank you.
Ken Martinez 1:22:14
Let’s make sure we have enough time to answer some questions from the audience. I’ll ask two more and then we’ll be mindful of the time as we move toward wrapping up the webinar.
First, a comment: Dr. Coleman—great work and excellent realization about the zoonotic risks in poultry.
And now a question: Can you tell us a bit more about the device and method you use for monitoring?
Kristen Coleman 1:22:36
Sure. In the study we conducted in Vietnam—and also in Malaysia—we used the NIOSH BC 251 bioaerosol cyclone sampler. I’ve used it in several different settings, and I’ve found it to be very reliable. So yes, that’s the device we used for bioaerosol monitoring.
Ken Martinez 1:22:57
Thank you. A follow-up question: Why are cats more vulnerable to HPAI than dogs?
This was asked in reference to a teenager in British Columbia who became seriously ill with HPAI and spent two months in the ICU. Before she got sick, her dog—who was later euthanized—was tested post-mortem for HPAI. So the question is really getting at the difference in susceptibility between felines and canines.
Kristen Coleman 1:23:19
That’s a really good question—and one I actually get quite often. I should probably defer to Dr. Baldwin on this one, since she’s a veterinarian. I’m not, and I don’t have a definitive answer.
Maggie Baldwin 1:23:33
Yes, thank you. Theoretically, dogs may be susceptible to some degree. But as to why we’re seeing so many more cases in cats than in dogs—I honestly don’t know. That’s likely a question best answered by a virologist.
Here in Colorado, we’ve tested a number of dogs, and to date, we’ve had no confirmed positive cases in canines. But we’ve had several positive feline cases—I believe we’re at about a dozen domestic cats so far—and we’ve also had cases among big cats.
Felines do seem to be particularly susceptible. But again, I would defer to someone with more specialized expertise in virology to explain why that is.
Kristen Coleman 1:24:18
It’s something I’ve discussed a lot with my PhD student. So maybe one day, he’ll help us figure it out.
Ken Martinez 1:24:28
Great, thank you both. Here’s another question: Has air sampling occurred inside indoor dairy or poultry facilities in Colorado? And has anyone implemented HEPA filtration or increased air changes in those facilities?
Maggie Baldwin 1:24:43
Excellent questions. So—I don’t know if this study has been published yet, and I’m not sure if the sampling was done on a farm here in Colorado—but someone associated with Colorado State University did conduct air sampling inside a dairy parlor. Interestingly, the results came back negative, which was surprising. That said, it was a sample size of one, and I don’t have full details about the specific setup.
This is something we discussed quite a bit last year—whether we could do broader air sampling for surveillance. We explored that idea. There was some concern from public health around implementing that kind of sampling. We also looked into existing programs like BioWatch, and ultimately concluded it probably wasn’t the best use of our resources at the time. But it remains an area of interest for us.
As for the HEPA filtration question—we’ve actually had one poultry facility inquire about it. This particular facility has been impacted by avian influenza three times, despite implementing incredible biosecurity measures. It’s a shower-in/shower-out facility. They’ve truly done everything we could ask of them.
The president of the company called me last year to ask about HEPA filtration and general air filtration options. Interestingly, he didn’t know that I’d worked on a similar project a couple of decades ago in Minnesota, related to PRRS virus oin swine farms. Back then, I worked with Dr. Scott Dee, who led research on enhanced biosecurity through air filtration in swine operations.
So, this poultry facility actually brought in a swine consultant to evaluate the feasibility of implementing similar filtration systems. It’s a large facility—housing up to 1.8 million birds—so we’re talking about a massive investment.
Whether it’s financially feasible is still uncertain. Even on smaller swine farms, it can cost millions of dollars. So the question becomes: is that level of investment worth it?
That said, one interesting development is the recent announcement from Secretary Vilsack about new federal initiatives. The administration is willing to offer up to 75% cost-sharing for producers who implement recommended biosecurity upgrades. I don’t believe HEPA filtration is currently included in those recommendations—but, hey, it might be worth proposing it.
Ken Martinez 1:27:09
All right, we’ve got about three minutes left. I’d like to close by asking each of you to share one sentence—or even just a word—that captures the most important action we can take to reduce risk from avian influenza at both the personal and public health level.
Let’s follow the same order: Dr. Baldwin, then Dr. Coleman, and finally Professor Mugavero.
Maggie Baldwin 1:27:31
Coordination.
I don’t even need a full sentence—just one word. Coordination between industry, public health, and all response partners is absolutely critical
Ken Martinez 1:27:45
Dr. Coleman?
Kristen Coleman 1:27:46
For the general public, especially regarding companion animals—awareness.
We really need to raise awareness that pets are vulnerable. If you notice symptoms or suspect your pet may have been exposed to avian influenza, let your veterinarian know immediately. Too often, diagnoses come after the animal has already passed—and I think we can do better than that.
Ken Martinez 1:28:19
Professor Mugavero?
Roberto Mugavero 1:28:22
Yes, I agree with Dr. Baldwin—coordination is essential. But I would add another word: cooperation.
Coordination is about structure and systems—but cooperation is about willingness. Too often, the missing piece is the genuine desire to collaborate. That’s the harder part. We must not only coordinate efforts but also foster a shared commitment to cooperation.
At the operational level, responders want to work together—we want to mitigate, to act, to prevent. But at the strategic level, among stakeholders and decision-makers, that cooperation must be intentionally cultivated.
So yes: coordination and cooperation.
Ken Martinez 1:30:05
Thank you, Professor Mugavero.
I want to extend a heartfelt thanks to our panelists today. This has been an incredibly rich and well-balanced discussion, offering diverse perspectives on how to approach and understand the challenges of avian influenza. I’d also like to give a special thanks to Venessa Sims, my co-moderator. She’s done a phenomenal job helping shape today’s panel and ensuring a thoughtful range of voices were included.
Before we wrap up completely, we’d like to take one final poll. We’re curious—are you aware of IBEC and the knowledge products we produce? Just a simple yes or no. Ala, could you please launch that poll now?
While the poll is running, I’ll go ahead and begin closing things out.
As many of you know, several of our most pressing endemic diseases—including influenza A and B and COVID-19—originated in animals before being transmitted to humans, often in connection with food production systems. That’s why IBEC’s next CLEAN Lessons Learned session will take a broader look at zoonotic diseases. We’re expanding beyond just avian influenza to better understand the full landscape of zoonotic threats.
From there, future webinars will explore additional emerging challenges, including the risks posed by shifting weather patterns and antimicrobial resistance.
If you enjoyed today’s webinar, I encourage you to visit our website at weareibec.org/events. There, you can find recordings of all our previous CLEAN Lessons Learned sessions, as well as other IBEC programming. All of these resources are free and available on demand.
For even deeper dives, check out our CLEAN segments from 2020–2022, which featured longer-format discussions and more extensive panels.
If you’re interested in getting more involved—perhaps even joining our Science Advisory Board—I invite you to reach out to me directly at kenm@weareibec.org. We’d love to hear from you.
A final thank you to Firebrand Creative for expertly managing today’s tech and to the American Industrial Hygiene Association (AIHA) for their unwavering support of this series.
To the volunteers and founding members who built and continue to power IBEC—your efforts are deeply appreciated and never taken for granted. We are a nonprofit and a volunteer-led organization, and we rely on support from our community. If you’re able to contribute—either personally or through sponsorship—please don’t hesitate to reach out. Your involvement makes a difference.
Together, we can continue advancing the mission of creating safer, healthier environments with lower disease burden and stronger, more resilient systems.
Thank you again for joining us—and we hope to see you at the next session. Take care, and goodbye for now.
Watch the other sessions of the 6-part IAQ CLEAN Lessons Learned series
The Critical Role of IAQ in Infection Prevention
Go to this sessionBridging the Gap Between Current IAQ Assessments and Evolving Biosensing Technologies in Built Environments
Go to this sessionVentilation as a Key Defense Against Infectious Diseases
Go to this sessionUnraveling Infectious Disease Transmission in the Built Environment
Go to this sessionIndoor Air Quality as a Public Health Strategy to Reduce the Risk of Infectious Disease Transmission in the Built Environment
Go to this sessionSponsor Spotlight

American Industrial Hygiene Association (AIHA)
AIHA is the association for scientists and professionals committed to preserving and ensuring occupational and environmental health and safety (OEHS) in the workplace and community. Founded in 1939, we support our members with our expertise, networks, comprehensive education programs, and other products and services that help them maintain the highest professional and competency standards. More than half of AIHA’s nearly 8,500 members are Certified Industrial Hygienists, and many hold other professional designations. AIHA serves as a resource for those employed across the public and private sectors and the communities in which they work.
Have a question about the event?
Connect with IBEC experts directly! Drop your queries below, and let's further the dialogue on preventing the spread of infectious diseases.