Watch the recording for a compelling discussion on IAQ, exploring effective strategies to mitigate infectious disease transmission in homes, workplaces, and other built environments
CLEAN Lessons Learned
Unraveling Infectious Disease Transmission in the Built Environment
Unraveling Infectious Disease Transmission in the Built Environment
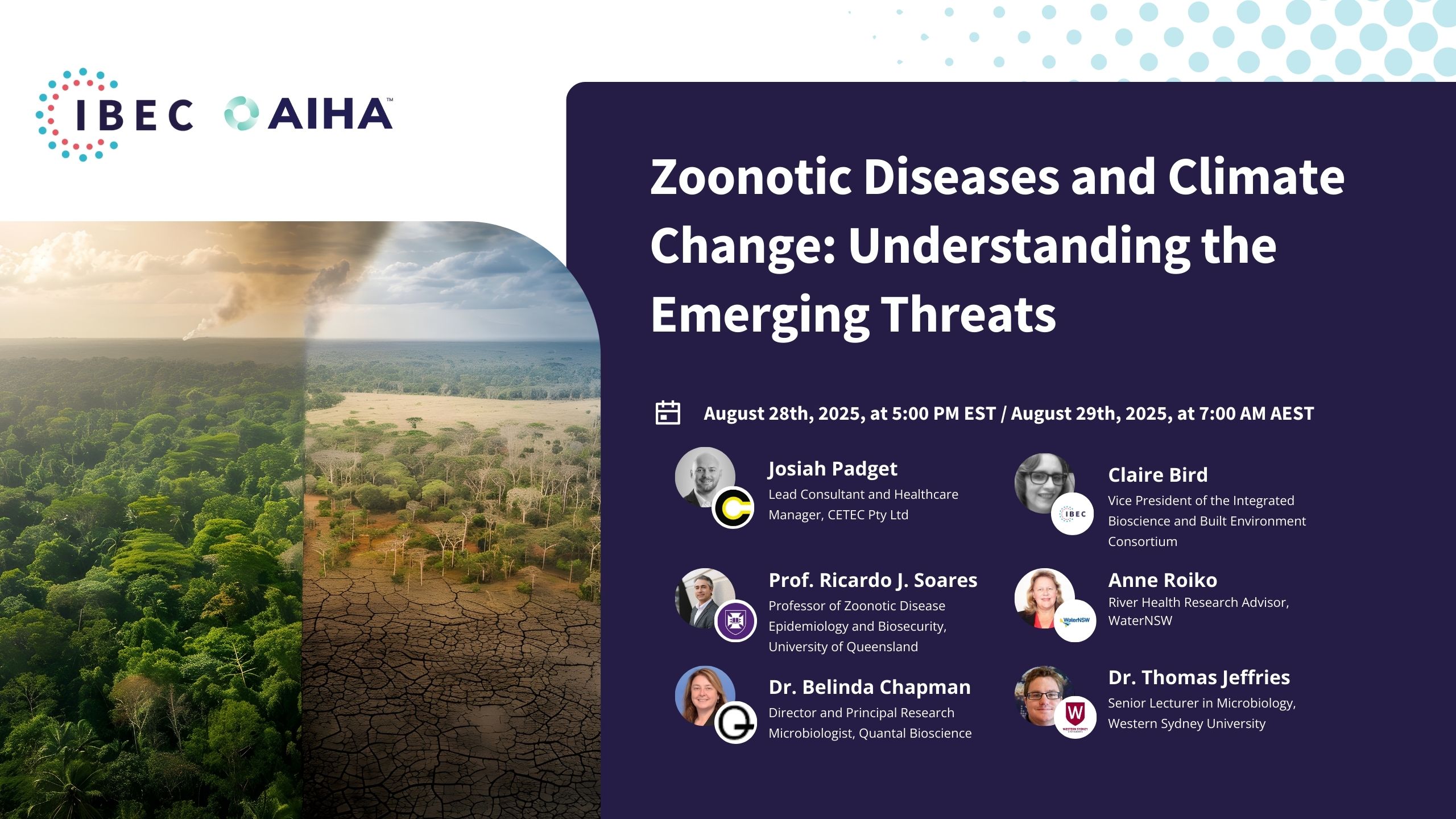
In the second of our four-part CLEAN Lessons Learned series dedicated to indoor air quality (IAQ) and its impact on infectious disease transmission in the built environment, we are shifting our focus to a topic of utmost importance: understanding the presence, risks, and ways to mitigate the spread of infectious disease in indoor spaces.
This session, sponsored by the American Industrial Hygiene Association (AIHA), is designed to bridge the gap between knowledge and practical application, ensuring that individuals are not only aware of potential threats in their environments but also equipped with strategies to address these challenges effectively.
Together, we will delve into infectious disease transmission in various built environments, comprehensively analyze potential hazards associated with these diseases, and provide you with practical information to protect themselves and their communities in various settings.
Joining the conversation, we’ll have expert panelists who bring their wealth of knowledge on air quality, bioengineering, microbiology, and occupational hygiene, representing organizations such as the National Institute for Occupational Safety and Health (NIOSH), the National Strategic Research Institute at the University of Nebraska (NSRI), the University of Nebraska Medical Center, Biosafety International, and McGill University.
- Interdisciplinary Collaboration: Collaboration among professionals from various sectors, including medical, engineering, and the agent sector, is vital for finding solutions to infectious diseases in buildings.
- Risk Management Approach: Implementing a risk management approach is crucial, where the level of risk is assessed, and building controls are justified based on the risk assessment.
- Engineering Controls: Effective and safe use of engineering controls, such as UVGI (Ultraviolet Germicidal Irradiation), is important. Multiple layers of protection, similar to safety measures in driving, are necessary for protecting against infectious diseases in buildings.
- Face Masks as Source Control: Face masks, particularly N95 respirators when properly fitted, serve as efficient filters and are effective as a form of source control to prevent the spread of respiratory aerosols.
- Ventilation and Filtration Synergy: Ventilation and filtration systems work best in conjunction with other measures, such as masks, to provide comprehensive protection against infectious diseases, both for close-range and longer-range transmission.
- Focus on Airborne Transmission: Airborne transmission is a significant concern, especially for respiratory pathogens like COVID-19. Mitigating airborne transmission is critical in indoor environments.
- Climate Change and Pathogens: Climate change is contributing to the emergence and spread of infectious diseases. It is driving changes in the distribution of pathogens, making previously inaccessible areas susceptible and increasing host vulnerability.
- Avoiding Dogma in Science and Communication: It’s essential to maintain open-mindedness and flexibility in scientific research and public health communication. Rigid adherence to dogma can hinder the ability to adapt to emerging evidence and communicate effectively during a rapidly evolving public health crisis.
- Cumulative Effect of Measures: Combining multiple interventions, including vaccines, masks, ventilation, and filtration, provides a cumulative effect in protecting against infectious diseases.
- Preparedness and Action: To address the challenges posed by climate change and emerging infectious diseases, proactive preparedness and collective action are necessary. It’s important to monitor environmental changes and adapt public health measures accordingly.

Kenneth Martinez
IBEC’s Chief Science Officer and Board founding member
Ken is an Environmental Engineer and Industrial Hygienist with experience in leading and conducting large-scale research, managing programs in occupational safety and health and emergency response; and creating and teaching professional development courses. He has over 33 years of CDC expertise in hazardous agent exposure characterization and mitigation control practices in the manufacturing and healthcare industry. Since retiring from the CDC, he served eight years in the CBRN space as a consultant focusing on a national biodetection program. Mr. Martinez is a recognized subject matter expert in biological agents, including infectious disease and bioterrorism agents.

Coby Gierke
IBEC's Executive Director
Coby Gierke is a distinguished leader with vast experience in numerous sectors. Currently, as Interim Executive Director at IBEC, he advances the Commit to C.A.R.E. program, securing endorsements from the CDC, AIHA, and the White House. He’s transformed educational events, introduced novel initiatives, and upheld regulatory standards. At Montana State Parks Foundation, Coby established key partnerships, managed finances, and initiated fundraising strategies, propelling the foundation to a prominent state role. Committed to personal and organizational growth, he’s attended several leadership trainings. Holding dual degrees from Portland State University, Coby’s leadership consistently instigates positive change, benefiting various organizations and communities.

Bill Lindsley, Ph.D.
Research Biomedical Engineer at the National Institute for Occupational Safety and Health (NIOSH)
Dr. Lindsley received his BS in Mechanical Engineering from the University of Maryland, College Park and his PhD in Bioengineering from the University of California, San Diego. He is currently a research biomedical engineer at the National Institute for Occupational Safety and Health (NIOSH), which is part of the Centers for Disease Control and Prevention (CDC). Dr. Lindsley studies the role of infectious airborne particles (called aerosols) in the transmission of diseases. He designed the NIOSH two-stage cyclone aerosol sampler which has been used to sample the air for airborne influenza virus, SARS-CoV-2 virus, and other pathogens. His group has collected coughed and exhaled aerosols from influenza patients and examined the amount of virus contained in these samples. Dr. Lindsley also designed the NIOSH respiratory aerosol simulator, which is used to study how well face masks and other face coverings block aerosols produced by coughing and breathing from being expelled into the environment and how well different measures like face masks, room ventilation and portable air cleaners reduce exposure to these aerosols.
Brett Cole
Managing Director and Chief Occupational Hygienist at Biosafety International
Brett is Managing Director/Chief Occupational Hygienist – Biosafety International/Member of Indoor Air Quality Association of Australia and Education & Training Committee (ETC) of Association for Biosafety for Australia and New Zealand.
Brett has been working in contamination control/hygiene in the High containment, Life Sciences, Healthcare, and Food/Beverage Market for over 20 years. His formal qualifications are in Environmental Microbiology & Chemistry and later in Occupational Hygiene and Toxicology.
His experience has been in Academic microbiological research, Medical device High-Level Disinfection, Engineering controls for contamination control in the built environment, materials handling, infectious and contaminated waste and facility microbial testing, decontamination, and remediation.
He has worked in Australia, New Zealand, Europe, North America, and Asia Pacific on many contamination projects from Beta-lactam site remediation for the Pfizer Vaccine Development, Research Animal Facility Infection, Pharmaceutical decontamination, Mould Infestation, Biological Contaminated Building decontamination.
In 2018, Brett wrote and presented the training material for the Safe use of Biological Safety Cabinets for the International Federation of Biosafety Associations (IFBA) and is a Certified Biorisk and Biowaste Professional with IFBA. He is also the lead Biosafety & Biosecurity Consultant to the PNG HIV and Malaria High Containment Facility in Port Moresby.
During the COVID-19 Pandemic, he has worked with two Federal Government Task Forces on PPE and Ventilators, IAQA Guidelines for Validation of Virally contaminated buildings as well as being the first International Contributor to a Technical Working Group on Decontamination for COVID-19 and a founding Contributor of IBEC.

Joshua Santarpia, Ph.D.
Science and Technology Advisor for the National Strategic Research Institute at the University of Nebraska & Professor of Microbiology and Pathology and Program Director for the Biodefense and Health Security graduate programs at the University of Nebraska Medical Center
Dr. Joshua Santarpia is Science and Technology Advisor for the National Strategic Research Institute at the University of Nebraska, the DOD-designated University Affiliated Research Center sponsored by U.S. Strategic Command.
Dr. Santarpia is a professor of microbiology and pathology and program director for the biodefense and health security graduate programs at the University of Nebraska Medical Center. He is also an adjunct faculty member in biological systems engineering at University of Nebraska–Lincoln where he leads the Collaborative Biosecurity Laboratory, a partnership between the Institute of Agriculture and Natural Resources and NSRI. He also directs NSRI’s independent research and development program and NSRI Fellows program.
Dr. Santarpia has held past positions at Edgewood Chemical and Biological Center and Johns Hopkins University Applied Physics Laboratory. He was most recently a distinguished staff member at Sandia National Laboratories.
Dr. Santarpia is trained in aerosol physics, atmospheric chemistry and microbiology. His peer reviewed research focuses largely on the fate biological aerosols in the atmosphere, detection of biological aerosols and atmospheric chemistry of biological and anthropogenic particles. He has contributed to several books on the characterization and measurement of biological aerosols in the environment.
Dr. Santarpia’s work is aimed at understanding and countering threats from biological organisms, especially those that pose a threat when dispersed in aerosols. He has worked extensively on RDT&E and OT&E efforts for biological sensors for both Department of Defense and Department of Homeland Security.
Much of Dr. Santarpia’s current work involves understanding the factors related to aerosol/airborne transmission of the SARS-CoV-2 virus.

Stephane Bilodeau, Eng., Ph.D., FEC
Adjunct Professor of the Bioengineering Department at McGill University and Chief Technology Officer at Smart Phases
Stephane Bilodeau has a unique background that combines academic, regulatory, and entrepreneurial experience. He holds a Ph.D. in Fluids Mechanics and Thermodynamics and a Master’s in Applied Sciences. Currently, he works as an Adjunct Professor in the Department of Bioengineering at McGill University and is the Chief Technology Officer in a Cleantech (Smart Phases).
He also serves as an Independent International Contractor for the United Nations Office of Project Services. With over 25 years of experience in research and development in clean technologies and solutions, Stephane actively contributes to various committees and task forces. He is the Chair of the Public Affairs Advisory Committee of Engineers Canada, Chair of the Covid Action Group, and Coordinator of the Indoor Air Quality Task Force at the World Health Network. Stephane is also one of the founding members of the Canadian Aerosol Transmission Coalition, where he actively contributes his expertise and knowledge.
Much of Dr. Santarpia’s current work involves understanding the factors related to aerosol/airborne transmission of the SARS-CoV-2 virus.
Coby Gierke 00:01
Hello and welcome, everyone. I’m glad you’ve chosen to spend your evening with us at IBEC, or morning if you’re in Australia or New Zealand. I’m very excited for today’s session, “Unraveling Infectious Disease Transmission in the Built Environment.” We have a great group of panelists and an interesting presentation for you. I want to start by thanking our sponsor, the American Industrial Hygiene Association (AIHA). The folks over at AIHA are sponsoring the Lessons Learned series, and we really appreciate their support. It takes funding and great partners like AIHA to help us get the word out and ensure the right people are in the audience for this session. So, a big thanks to Larry and his team at AIHA.
For those unfamiliar, my name is Coby Gierke, and I’m the Executive Director of IBEC, the Integrated Bioscience and Built Environment Consortium. We are a 501(c)(3) nonprofit organization based in the United States. We started in 2020, at the beginning of the COVID pandemic, and have been working since then to understand how people, pathogens, and buildings interact. We aim to work across disciplines to decrease the transmission of infectious diseases and make it safer for people to congregate indoors.
IBEC does a number of things, including programs like Lessons Learned. We have a robust membership program, and we have a great group of scientific advisors that meet regularly to review what’s happening in the industries of people, pathogens, and buildings. We’ve had success with our CLEAN Summits and the Lessons Learned series, an extension of those summits. We’ve also had success with the program called Commit to C.A.R.E., another partnership with AIHA. We recently received news that Commit to C.A.R.E., which can be found at www.commit2care.org, is being endorsed by NIOSH and will be linked on their website. We’re excited about that and the 20-plus partners that have signed on to be Commit to Care partners.
Finally, I’ll mention that we recently were awarded funding from the CDC Foundation here in the US to develop knowledge products addressing a potential resurgence in mpox. Our goal is to prevent that resurgence and distribute these knowledge products to the right community leaders in vulnerable communities.
I’m always happy to share more information about IBEC’s work. You can reach me at cobyg@weareibec.org. I also want to thank the many IBEC members attending today’s session. IBEC is a membership-driven organization, and we value our members’ support. For those who have renewed their membership for 2023 and 2024, we appreciate it. For those not yet members, I encourage you to consider joining IBEC. We have affordable options for individuals, businesses, and institutions. You can learn more at our website, weareibec.org.
With that, I want to introduce our moderator for today, IBEC’s Chief Science Officer, Ken Martinez. Ken, the floor is yours. Thank you.
Kenneth Martinez 04:11
Thank you, Coby. Welcome to the second in this series of IBEC lessons learned, focusing today on unraveling infectious disease transmission in the built environment. All of these sessions are available on our website, as Coby mentioned: weareibec.org. You can watch earlier ones and acquaint yourself with the different topics we’ve focused on. For this four-part series, we’re focusing on indoor air quality and its connection with infectious disease transmission. The third session will be in a couple of months, focusing on ventilation in the built environment, where we’ve already targeted some outstanding speakers. The last one will focus on indoor air quality metrics and how they relate to or can help during a pandemic or an infectious disease outbreak.
Today, we’ll hear from a second group of experts providing ongoing information on controlling airborne infectious agents. This session will focus on two key components: first, on infectious disease research and controlling pathogens, and second, on monitoring and managing them to reduce disease transmission. We have an international perspective, with one panelist from Canada and another from Australia. Welcome to those joining us internationally.
These experts bring capabilities that span infectious diseases, including how they spread, how to reduce their spread, and what to consider in preventing their spread in the built environment. Each panelist will give a 10-minute presentation, followed by a directed question. After all presentations, I will ask a series of questions, then we’ll shift over to a Q&A. Please put your questions in the chat room. This session will be recorded for later viewing.
As far as IBEC is concerned, and as Coby gave an excellent introduction, we’ve always focused on three things: buildings, pathogens, and people, especially during the pandemic. While medical diagnostics and vaccination are crucial, we also discuss issues related to the built environment and how people react to the pandemic, incorporating building behavioral sciences, engineering, ventilation, and environmental microbiology. We’ll also discuss the role of mechanical air handling systems and supplemental technologies in their control. IBEC aims to provoke active industry discussion, so please share your comments and questions in the chat box.
We have a social lounge available after this session for those who want to stay and converse with others. Now, let’s move on to our panel. We welcome Dr. Joshua Santarpia, Dr. Bill Lindsley from NIOSH, Brett Cole from Australia, and Dr. Stephane Bilodeau from Canada.
I’ll start by introducing Dr. Joshua Santarpia. Dr. Santarpia is a full professor of microbiology and pathology and program director for the bio defense and health security graduate programs at the University of Nebraska Medical Center. He’s also an adjunct faculty member in Biological Systems Engineering at the University of Nebraska Lincoln, where he leads the Collaborative Biosecurity Laboratory, a partnership between the Institute of Agriculture and Natural Resources and the National Strategic Research Institute. He directs NSRI’s independent research and development program and the NSRI Fellows Program. Dr. Santarpia’s work is aimed at understanding and countering threats from biological organisms, especially those that pose a threat when dispersed in aerosols. His research includes characterization of biological agents, environmental microbiology, and atmospheric chemistry of biological aerosols. He has contributed to several books on the characterization and measurement of biological aerosols in the environment. His current research involves how biological aerosols interact with reactive atmospheric compounds and biological sensors. He has worked extensively on the recent development and testing, evaluation, and operational testing development of biological sensors for both the Department of Defense and Homeland Security. Josh, I’m turning it over to you.
Joshua Santarpia 09:23
Thank you. Today, I’m going to address a source of frustration for me throughout the pandemic. My primary motivation stems from the fact that my group was among the first to measure SARS-CoV-2 in aerosols. Despite this, it took the WHO and other public health organizations two years to acknowledge that COVID-19 is airborne. As a scientist collecting data on the ground, this was incredibly frustrating, particularly feeling that our findings were not fully believed.
By March and April of 2020, there was significant evidence of SARS-CoV-2 RNA in aerosols globally. By late spring and early summer of 2020, multiple groups, including ours, had evidence that aerosols containing SARS-CoV-2 could replicate in cell culture. By mid-2020, there was evidence of aerosol transmission of SARS-CoV-2 between animals. This wasn’t just one piece of evidence; it was a multitude of findings indicating that COVID-19 was airborne.
I believe a fundamental issue was the dogmatic bias in the medical community regarding droplets and aerosols, particularly the artificial dividing line around five microns. Data had shown that particles smaller than five microns carried COVID-19, yet there was still debate about transmission. This suggests a lack of understanding of aerosol science, which, until 2020, was a niche field not widely understood outside of specific circles. Despite rapid technological developments, there are no accepted community guidelines for best practices in aerosol sampling, leading to uncertainty and varied interpretations of data.
In terms of technological approaches, I advocate for making aerosol samplers smaller, quieter, and less expensive. Smaller and quieter samplers can be used in various settings like hospitals and schools without being intrusive. Reducing costs makes these samplers accessible for use in low-resource environments, crucial for early detection and characterization of diseases.
Regarding guidelines and best practices, a rigid set of best practices might be counterproductive by limiting the types of technologies and methodologies that can be used effectively. Every aspect of the sampling process needs to be characterized, including sampling parameters like flow rates and collection efficiencies. This characterization is vital for making data comparable across different instruments and settings.
A significant technological advancement needed is the development of methods to determine the threat of an organism without relying on culture. The current gold standard for assessing infectiousness is culturing the organism, but we need alternative methods that can quickly and effectively determine the hazard potential of an organism.
Community guidelines are crucial. We need to define what constitutes a hazard in a measurable and definitive way, setting the minimum and maximum thresholds for what we consider an airborne transmissible component. This clarity will enable positive recommendations and better preparedness for future pandemics.
To conclude, I emphasize the need for smaller, cheaper aerosol samplers, understanding and optimizing sample preparation, and community guidelines to define hazards. Addressing these areas will significantly advance our ability to manage and mitigate airborne infectious diseases.
Kenneth Martinez 21:45
Thank you, Josh. That was indeed powerful. I’m going to use my moderator’s prerogative to change the question I originally planned to ask you. Initially, I had a different line of inquiry, but your compelling presentation rendered that irrelevant. You were actively involved in the COVID-19 response, particularly with the cruise line industry, through your work at the University of Nebraska. Historically, emerging infectious disease events are primarily a public health focus, where public health entities take the lead. Coming from an environmental microbiology and aerosol science background, how did you integrate yourself into this role with the response team? And how did you leverage your expertise to effect change in the response strategy?
Joshua Santarpia 22:31
Yes, that’s a story I’m particularly proud of. In fact, I had been working with our biocontainment unit for several years prior, focusing on hazards in medical transport and healthcare environments. Around December 2019, they approached me regarding a novel respiratory disease emerging in China. They anticipated the repatriation of US citizens and wanted to assess their readiness for handling airborne diseases, as they had not dealt with such in the past. They requested my assistance in evaluating their protocols and conducting tests.
To directly answer your question, I made myself available to assist the medical community as much as possible. Having already established a collaborative relationship, they trusted the measurements and experiments I conducted. When patients arrived, we were fully prepared to implement tracer-type experiments in the hospital.
Regarding effecting change, Nebraska Medicine and UNMC have a strong collaborative ethos. When we presented our findings on aerosol transmission, instead of reducing protective measures based on WHO or CDC guidelines, the hospital system took our data seriously. They focused on mask reuse protocols rather than diminishing masking requirements. As a result, for the entire first year of the pandemic, we had zero nosocomial transmission of COVID-19 among healthcare workers, a significant achievement that wasn’t common everywhere. This outcome reaffirmed the importance of our collaborative approach and the trust built within our medical community.
Kenneth Martinez 25:38
It really is. I recall from my time at the Centers for Disease Control and Prevention (CDC), responding to the North York General Hospital, which was their SARS outbreak hospital. Half of the patients in the SARS ward were healthcare workers, nurses. So yes, I concur with you. That is huge. All right, we’re going to move on. We’ll have more time for conversation. So I’d like to introduce our next speaker. He is Brett Cole, and he is from Australia. Brett operates a business providing international services in contamination control in high containment facilities for a wide range of government, universities, building operators and managers, and also the healthcare sector. Stemming from a background in environmental microbiology and chemistry, and later in occupational hygiene and toxicology, he has worked across academia, medical devices, high-level disinfection, hazardous materials, and waste management, and assessment of microbial contamination. Brett has recently been appointed to the board of the Association for Biosafety Australia and New Zealand (ABSANZ) and is a highly active member of the IBEC Scientific Advisory Board and also part of our Board of Directors. Brett, would you like to tell us a bit more about yourself and how you hope to contribute to the discussion today?
Brett Cole 26:49
Thank you, Ken. And thank you to IBEC for the opportunity to speak amongst such an esteemed group. My background, as Ken pointed out, is largely in the built environment and infectious risk, particularly in high containment, well-controlled environments. This includes healthcare settings, pharmaceutical life sciences, high containment BSL Level labs, and the food and beverage industry. Like all of us, during COVID, we were called to action to serve the community in more commercial and residential settings as well.
I’d like to highlight some of the mechanisms involved in infections and transmission in the built environment. This is multi-modal, encompassing not just airborne routes, but also the potential for water-based infection. My focus is on biological risk agents, considering exposure routes and potential hazards in the work environment. I’ll share some slides here to further illustrate these points.
[Proceeds to present slides]
These slides, including system drawings from ASHRAE 241, show the complexity of airborne systems and format transmission in the built environment. We see the interplay of various components like mechanical systems, natural ventilation, and surface contamination. It’s crucial to understand these complex systems and their interactions, not only within a room but across entire buildings.
In Occupational Hygiene, we focus on exposure routes and hazards. Biological risk agents are a particular concern, and we often revert to the hierarchy of controls, which includes elimination, substitution, engineering, administration controls, and PPE, to manage these risks. During COVID, we saw an inversion of this hierarchy, with a heavier reliance on PPE due to limitations in other control areas.
Balancing the hierarchy of controls with Maslow’s hierarchy of needs is essential. Human reactions and compliance with regulatory frameworks can significantly impact the effectiveness of control measures.
In controlled environments like high containment labs, we still see breaches and infections despite strict controls. This highlights the need for effective containment strategies close to the source of hazards. Understanding the building’s functionality and occupant behavior is key to implementing effective controls.
Lastly, infectious risks in the built environment are not limited to airborne transmission but also include surface (fomite) and water transmission. We must employ various levels of controls, tailored to specific environments and situations, to effectively mitigate these risks.
Kenneth Martinez 41:37
Thank you, Brett. I have a question for you. Given that you deal with or advise on highly pathogenic microorganisms in your work, can you tell us what makes one pathogen more dangerous than another? Additionally, can you explain how this might affect your response to an outbreak of an infectious disease?
Brett Cole 41:55
Certainly, Ken. Key to managing any outbreak or infection is understanding what you’re dealing with. The old adage applies: you can’t win the fight if you don’t understand it. So, being able to rapidly diagnose the pathogen and understand its epidemiology, whether it’s airborne or surface-borne, is crucial. Regarding whether one poses a greater risk than others, I think it depends on the context. During COVID, obviously, the airborne risk was much greater compared to the research around fomite transmission of COVID. But it’s also important to remember that what is airborne can eventually fall to surfaces. Therefore, good hygiene practices, both in terms of building air handling and ventilation as well as surface cleanliness, are critical. The research from Australian hospitals indicated that stewardship, including environmental hygiene and cleaning, led to decreased infections and reduced hospital stays. So, understanding the pathogen, measuring its presence, and then employing mitigation strategies using both existing building features and additional measures are key. Then, ensuring these strategies are effective through measurement is crucial. It’s important to recognize these are complex systems, thus stakeholder engagement and understanding are fundamental to successful outbreak management.
Kenneth Martinez 43:24
Thank you, Brett. Now, it’s my honor and privilege to introduce our next speaker from the National Institute for Occupational Safety and Health (NIOSH). He is Dr. Bill Lindsley. I’ve had the honor of working with Bill in the past when I was with NIOSH for 33 years. Dr. Lindsley received his Bachelor of Science in Mechanical Engineering from the University of Maryland in College Park and his Ph.D. in Bioengineering from the University of California in San Diego. He is currently a Research Biomedical Engineer at NIOSH, which is part of the Centers for Disease Control and Prevention (CDC). Dr. Lindsley has studied the role of infectious airborne particles, known as aerosols, in the transmission of diseases. He designed the NIOSH two-stage cyclone aerosol sampler, which has been used to sample airborne influenza virus during the H1N1 pandemic, and more recently for the COVID-19 pandemic in sampling for the SARS-CoV-2 virus, as well as other pathogens. His group has collected cough and exhaled aerosols from influenza patients and examined the amount of virus contained in these samples. Bill also designed the NIOSH Respiratory Aerosol Signature Simulator, which is used to study how well face masks and other face coverings block aerosols produced by coughing and breathing from being expelled into the environment, and how well different measures like face masks, room ventilation, and portable air cleaners reduce exposure to these aerosols. In a recent publication, Bill stated that portable air cleaners can be used to reduce indoor exposure to infectious airborne pathogens, wildfire smoke, allergens, and other hazardous aerosols. However, during public health emergencies such as the recent COVID-19 pandemic, the need for air cleaners can greatly exceed the available supply and federal financial resources. He then discusses how we might overcome these issues at a time of such shortages. Welcome, Bill.
Bill Lindsley 45:41
Okay, sorry again, just having a little bit of difficulty here. Okay, thank you very much. I’d like to run through an example of some research we conducted during the pandemic to give a sense of what we did and how we did it. As we now know, SARS-CoV-2 spreads mainly by aerosols. When people cough, sneeze, speak, or even just breathe, they exhale infectious particles, which others inhale, causing infections. One way to reduce this is by filtering those particles out of the air before they cause infection, commonly done using portable air cleaners. These have several advantages: they are quick and easy to add to a room, flexible, don’t require changes to building ventilation, and filter out other aerosols like pollen and soot. However, they can be expensive, and there can be shortages during public health emergencies. Consequently, many people in the US have used Do It Yourself air cleaners, building their own, often at a lower cost and with widely available materials, such as box fans and standard HVAC filters.
The most popular DIY design in the US is the Corsi-Rosenthal box, which consists of four MERV 13 filters taped together to form a box with a box fan taped at the top. Air is pulled into the filters and blown out the top by the fan. To test these, we used a simulated meeting room or classroom equipped with four breathing robots, one emitting cough or exhale aerosols, and the others breathing. This setup helps simulate an infected person in the room, and we can monitor how much aerosol reaches the other robots.
Our room, roughly the size of a typical classroom, had two Corsi-Rosenthal air cleaners, one at the front and one at the back. We controlled the room ventilation at two air changes per hour, typical for a US classroom. Our findings showed that these DIY air cleaners could reduce respiratory aerosol exposure by 50% to 78%, comparable to commercial air cleaners. However, a significant issue with DIY air cleaners is the lack of quality control. While commercial air cleaners are often tested and certified, DIY versions may have design or construction flaws like leaks or gaps, or use poor-quality filters, all of which can significantly reduce performance. Unfortunately, there’s no easy way for the average person to test the effectiveness of their DIY air cleaner.
In summary, that’s a brief overview of our work during the pandemic, and there’s more detailed information available in our published research. I’ll hand it back over to you, Ken.
Kenneth Martinez 52:13
Thank you, Bill, for that perspective on NIOSH research. That was excellent. So, a question for you: Your design of the two-stage cyclone, which we didn’t get to talk about here, but was novel and impactful, particularly in the application of sampling for airborne agents of concern. What are some of the key points that resulted from your successful sampling of influenza and SARS-CoV-2 from the air?
Bill Lindsley 52:36
We learned a couple of good lessons from our research. Probably the most significant lesson is that sampling airborne viruses is a lot harder and more complicated than you might think. Airflow in a room is complex, and how the virus is emitted varies significantly from person to person. Consequently, you see substantial differences in concentration even between samplers located just six feet apart. Over time, the concentration also fluctuates extensively. For instance, if someone infected enters a room, the concentration spikes, then drops significantly when they leave.
The key takeaway is the importance of carefully planning your sampling strategy and collecting as many samples as frequently as possible. Often, the findings can be surprising and may not align with initial expectations.
Another observation that has repeatedly come up in our research is that the vast majority of airborne virus sampling, both before and during the pandemic, utilized PCR to detect the virus. PCR is excellent for identifying the genetic fingerprint of a virus, but it also works on non-viable viruses. This means that while we’re detecting the virus, we can’t confirm if it’s infectious.
Moving forward, there are emerging designs that help preserve the infectivity of the virus. This shift in research methodology is moving from solely using techniques like PCR to more advanced techniques that assess infectivity, thus demonstrating not just the presence of the virus but also its potential hazard and impact on people.
Kenneth Martinez 54:48
Thank you for that answer. Alright, we’re going to move on now. I’d like to take the honor of presenting Dr. Stephane Bilodeau. Dr. Bilodeau is an engineer with a PhD in Thermodynamics and Fluid Mechanics and a Master’s in Applied Sciences. He is an Adjunct Professor in the Department of Bioengineering at McGill University and an Independent International Contractor for the United Nations Office for Project Services. He is also the Chief Technology Officer for Cleantech Markphases. Both an academic and an entrepreneur in clean technologies for more than 25 years, Dr. Bilodeau is the Chair of the Public Affairs Advisory Committee at Engineers of Canada. He’s also the Chair of the COVID Action Group and the Coordinator for the Indoor Air Quality Task Force at the World Health Network. Additionally, he actively contributes to the Canadian Aerosol Transmission Coalition. Dr. Bilodeau, we look forward to hearing your presentation and the part you play in today’s discussion.
Stephane Bilodeau 55:48
Thank you for the kind introduction. Let me share my screen for a few seconds, I’ll try to do it the proper way. It should be coming up. As I mentioned, thank you for this introduction. I’m actively involved in groups like the Canadian Coalition for Airborne Transmission, and the WHN, which are taking indoor air quality and discussions related to minimizing the risk associated with airborne disease very seriously. Indoor air quality is a crucial aspect of ensuring the health and safety of residents, staff, visitors in a building, from schools to care homes, from offices to hospitals. The COVID-19 pandemic has highlighted the importance of indoor air quality in preventing the transmission of airborne disease. In addition, the wildfires in 2023 have raised concerns about the intrusion of outdoor contaminants into indoor air, adding to the health risks. Today, I will discuss more about how to mitigate these risks and improve air quality in the built environment.
First, clean air is a human right. Let’s start with this significant milestone two years ago, on October 8, 2021, when the Human Rights Council declared that having a clean, healthy, and sustainable environment is a human right, including air quality. Air pollution alone was responsible for around 6.5 million premature deaths, as published in The Lancet just last year, 8.2 to 8.7 million in 2018-2019, from data reported by WHO. And on top of that, we could add airborne transmitted COVID-19, which also was responsible for more than 7 million officially reported deaths in the last three years, and certainly more.
I will not dwell much on tiny particles, the aerosols, as my outstanding colleagues have already discussed that in great detail. But all these aerosols and contaminants, including airborne disease, or pathogenic microbes, various bacteria, or viruses like COVID, come with different levels of risks. Dealing with the risks is always about evaluating and addressing this level.
I’ll quickly jump over these next two slides about airborne disease. COVID is a bad example, but there are many others like chickenpox, common cold, tuberculosis, which are airborne in nature. These are carried by tiny droplets and microdroplets, which we call aerosols.
Wildfires, as Bill mentioned, are also a concern. Studies have shown that air pollution and wildfire smoke can increase mortality from COVID. People living in areas with air pollution face an increased risk of mortality from COVID. So, improving indoor air quality can help not only with airborne disease but also with other types of contaminants.
There are many factors and tools that affect indoor air and airborne transmission in buildings, including air flows, patterns, types of ventilation, air filtration, disinfection, and indoor CO2 level monitoring. Let’s dive into some of the guidelines and standards. While there are good standards already, such as ASHRAE 62.1, which focuses more on particles and gas control and not much on pathogens, it is important to understand whether “acceptable” is sufficient and if we should aim for good practices.
ASHRAE 241, which addresses aerosol infection control in healthcare spaces, offers higher protection in some spaces. It specifies air changes per hour, indoor-outdoor air supply levels, and recommends HEPA filtration. But what about using healthcare standards in other buildings, not only hospitals?
Monitoring indoor air quality is crucial. CO2 monitoring can be a good proxy for ventilation levels. If CO2 accumulates in a building and goes beyond optimal levels (600-800 ppm), it can increase the risk of airborne transmission. This is higher than the regular standard of 1000 ppm.
Other solutions include HEPA filtration, UVGI systems, and far-UVC, which reduces risks for skin damage or cataracts. However, they must be implemented by professionals and maintained properly.
Just as concluding remarks, I would like to focus on three significant aspects. Firstly, multidisciplinarity is crucial. Approaching solutions with a multidisciplinary mindset is essential, involving facility managers, public health advisors, occupational health and safety specialists, engineers, etc. This is something we’ve strived to apply in the Airborne Coalition and a regional coalition in Canada, with professionals from the medical sector, engineering, and the agent sector contributing to finding appropriate solutions. This is vital when dealing with infectious diseases in buildings, as we face complex problems, systems, and solutions. It’s crucial to understand that no single specialty or type of expert can find the ideal solution alone; we need input from various backgrounds and areas of expertise.
The second point to remember is the importance of a risk management approach when finding solutions. Consider the level of risk, evaluate it, make an assessment. It’s crucial to establish building controls justified by the risk assessment. Facility managers know resources are limited, so it’s important to choose tools that provide the most significant impact on protection, thereby minimizing risk. This approach is applicable everywhere, from homes to hospitals and offices, tailored to the resources available and the level of risks faced.
Finally, the effective and safe use of engineering controls is important. I referred to risks associated with tools like UVGI (Ultraviolet Germicidal Irradiation). If applied correctly, they can achieve the desired outcomes. However, engineering controls are not the sole solution. Think in terms of multiple layers of protection. In driving, we have seatbelts, airbags, and brakes; similarly, when protecting against infectious diseases in buildings, we need multiple layers. This built environment requires a combination of solutions, as I briefly mentioned in the slide. Are you ready? There are compelling reasons to adopt more stringent healthcare standards in various buildings, not just in hospitals. So, do not hesitate to promote and use these Indoor Air Quality (IAQ) best practices. Thank you.
Kenneth Martinez 1:17:04
Thank you, Stephane, you have indeed answered my question that I had noted down. Given the importance of time, I would like to bring all the panelists back online. I am planning to focus on the Q&A questions coming from the audience. I want to inform you all that we have been attempting to respond to these questions online wherever possible. There is one particular question I would like to direct to Billingsley, and then I will proceed to ask a few more questions based on my own notes. Brett has already addressed one question from a participant regarding whether we should consider patients as mobile sources of aerosol transmission. A follow-up question for Bill is, if patients are considered mobile sources, do face coverings act as an engineering control for source control? Additionally, Bill, I’d like your input on Dr. Ken Mead’s work, which you might be familiar with. He created a ventilation system for patients with potentially airborne infections, aiming to exhaust whatever they are emitting.
Bill Lindsley 1:18:04
Yes, to address your first question, absolutely, face masks are indeed a form of source control. They are probably more effective as source control devices than they are for personal protection. This is because they serve as efficient filters, particularly when people cough or exhale through a well-fitting mask. During the pandemic, we conducted several tests and published papers demonstrating that face masks are highly effective at source control. We found that the best device for controlling respiratory aerosols is the N95 respirator, especially when it fits properly. A good fit prevents facial leaks and ensures effective filtration. However, there are drawbacks to using face masks. Firstly, people generally dislike wearing them, and secondly, in cases where a patient is already experiencing distress, it’s preferable to avoid putting a face mask on them. This is where Dr. Ken Mead’s airborne isolation system becomes highly effective. It works by pulling air past the patient and filtering it, thereby preventing the patient from contaminating the environment without requiring them to wear a face mask.
Kenneth Martinez 1:19:17
Thank you, Bill. Josh, this question is directed at you and comes from one of our participants. They mentioned that you are at a university that conducted some of the early work in meatpacking plants. Were you involved in this effort? And if so, in what capacity?
Joshua Santarpia 1:19:30
Yes, there are a couple of aspects to that question. Initially, some of the first assessments we conducted were focused on the meatpacking industry, which was significantly affected by COVID-19. Meatpacking is a major industry in Nebraska, so our team conducted in-person assessments at many of these facilities. While I was not directly involved in those assessments, I did consult on some of the recommendations that were included in the playbooks. In 2021, we began conducting in-situ exposure assessments in some of these meatpacking plants, specifically looking at exposure to human aerosols. The findings and recommendations from these assessments were shared directly with the unions and the industry. We are currently in the process of preparing publications on this work.
Kenneth Martinez 1:20:25
Thank you, Josh. We have a new question from the audience that I believe would be relevant for Bill, Brett, Stefan, and even Joshua to weigh in on. The question is: Are ventilation and filtration systems sufficient to operate independently of masks and respirator masks, or are they intended to function in conjunction with one another? This inquiry pertains to both close-field transmission and longer-range transmission.
Bill Lindsley 1:20:48
I’ll attempt to address that first. We’ve found that, particularly in terms of short-range transmission, nothing is as effective as a face mask. It’s simply not feasible for a ventilation or filtration system to remove aerosols quickly enough if someone is coughing or breathing directly in your face from just three feet away. We also discovered that all these interventions are most effective when used together. If you combine masking with a filtration system and enhance the HVAC (Heating, Ventilation, and Air Conditioning) system, the combined effect gives a much better result than using any one method alone.
Brett Cole 1:21:25
I completely agree with Bill. It’s easy to examine controls individually and question which one is more effective than the others. However, there’s a synergistic effect. As I presented and as Bill mentioned, Personal Protective Equipment (PPE) became our first line of defense in mitigating close-range infectious risks. Subsequently, portable air cleaners, HVAC, and other technologies work in conjunction. It’s about containing the microbiological risk as close to the source as possible, and nothing works better than a mask, as Bill pointed out, to protect not just the individual but the community from infection.
Stephane Bilodeau 1:22:09
If I may add, it’s about the multi-layer approach I mentioned a few minutes ago. That’s crucial. I used the car example earlier. You need multiple layers of protection because if one fails – even if masks are perfect, people are not and might remove them occasionally – the ventilation can cover for other lapses. So, it’s vital to have multiple layers for effective protection, not just one. Ventilation is a part of it, and PPE is another important level of protection.
Joshua Santarpia 1:22:55
Okay, I’ll just add my agreement with everyone here. Fundamentally, all of our interventions are designed to work in conjunction, not in isolation. Solely getting a vaccine or just wearing a mask doesn’t provide complete protection. It’s the combination of everything that works together effectively. In the beginning, we saw it as a game of inches, gaining incremental benefits with each added intervention. So, remember, it’s the cumulative effect of these measures that’s important.
Kenneth Martinez 1:23:33
I would like to direct my next question to both Brett and Josh. Brett, you discussed the two modes of transmission: airborne versus fomite transmission. You touched a bit on which is more problematic, and I think, Josh, you emphasized this in your discussion. How do we more effectively communicate that airborne risk is significantly higher? I say this because a colleague of mine from the Centers for Disease Control and Prevention (CDC), who was an anthrax expert, once told me to consider how our bodies are designed to keep pollutants out. We blink our eyes to remove things, and we have nasal hairs to stop large particles from entering. However, what we inhale, particularly if it reaches the alveoli, the air sacs in our lungs, is essentially an open window to our bloodstream. Could you both discuss this issue and elaborate on it?
Brett Cole 1:24:27
Yes, definitely. I’ll refer back to one of the earlier questions which highlighted the importance of understanding the epidemiology of the pathogen. From a respiratory standpoint, diseases like COVID-19 pose a far greater airborne risk than surface risk. In the early stages of the pandemic, there was significant focus on the fomite transmission of COVID. Numerous studies examined its robustness and longevity on different surfaces. However, we should remember that COVID-19 is a respiratory ailment, a virus of the respiratory tract, and it will become airborne at some point. Therefore, risk mitigation should focus more on airborne transmission than surface transmission. Although some virus particles will settle on surfaces, good hand hygiene and environmental cleaning can greatly mitigate this risk. In my opinion, the airborne aspect is the most critical to mitigate.
Joshua Santarpia 1:25:35
Yes, I agree that for respiratory pathogens, this is certainly true. However, it’s important to remember that the mode of transmission greatly depends on the specific pathogen we’re dealing with. While there’s been a focus on COVID-19 for obvious reasons over the last three years, it’s not the only pathogen of concern. It’s crucial not to neglect other hygiene practices, like hand washing, to prevent other diseases. We also shouldn’t forget to clean surfaces, as neglecting this can lead to the transmission of other diseases. The transmission modes aren’t universal. Over the past three years, we shouldn’t come away with the idea that protecting only the respiratory tract is sufficient. This might not be a realistic assumption in the built environment. While many pathogens might have an unrecognized aerosol route of transmission, we must be careful not to overlook the variety of other ways that pathogens can be transmitted.
Kenneth Martinez 1:26:52
Thank you, Bill. I have a question that I think is most suited for you. I am interested to know if there is progress in developing and possibly reaching an agreement between agencies on a standardized method for measuring the effectiveness of face coverings as a source control. Is there any work being done by the National Institute for Occupational Safety and Health (NIOSH) or elsewhere on this?
Bill Lindsley 1:27:11
There is indeed a lot of work being done in this area. Currently, ASTM International has formed a working group that is endeavoring to establish a standard for precisely this purpose. So yes, there is ongoing work aimed at devising a universally agreed-upon standard for testing. These processes are complex and take time, but such a standard is in development.
Kenneth Martinez 1:27:31
Alright, we have time for one more question. I will use my discretion to ask this, as I believe it’s a fitting conclusion to our discussion. I want all four of you to address the topic of atmospheric science and its intersection with airborne pathogens. We have stated that climate change may be driving an increase in hard-to-treat infectious agents. For example, in the United States, we are now witnessing an upsurge in malaria cases in the South, leprosy cases in Florida, and a case of blastomycosis in a paper mill in the Michigan area, which has never been seen before, according to a NIOSH investigator’s research. I’d like your perspectives on how climate change will prompt us to become more aware of emerging infectious diseases.
Brett Cole 1:28:21
If everyone is comfortable with me starting, I believe climate change and climatic conditions, particularly increased environmental humidity and similar factors, are playing a role. We’re observing that environments in the U.S., both southward and northward, which were previously inhospitable for diseases like tuberculosis and other stubborn bacteria, are now becoming suitable for their spread. These changes are likely linked to global warming. It’s challenging to examine these issues in isolation, but there’s a discernible trend. My PhD research and other studies indicate that global warming is significantly influencing these shifts, along with factors like antimicrobial resistance. This is definitely an area that merits close attention and is likely to pose ongoing challenges.
Stephane Bilodeau 1:29:24
I’d like to add my perspective. Climate change and global warming are affecting two aspects of this issue. Firstly, as you mentioned, new pathogens are gaining access to communities that were previously inaccessible to them. Secondly, these climatic changes are making people and communities more vulnerable. A study from the TC Chen School of Public Health indicated that air pollution could increase the severity of diseases, with an 11% increase in mortality among people affected by long-term air pollution exposure. This vulnerability is compounded by the increasing frequency of wildfires, droughts, floods, and other environmental crises, which are already impacting people’s health. With the addition of new pathogens accessing these more vulnerable communities, we are potentially facing a heightened risk scenario in the future, especially given that global warming shows no signs of abating soon.
Joshua Santarpia 1:30:48
Yeah, Stephane and Brett have already touched on many points I would have mentioned. One key aspect is the emergence of zoonotic diseases, which occurs when humans interact closely with the untamed natural world. As we venture into places previously unexplored and interact with species we’ve never encountered before, opportunities arise for pathogens to jump species. Climate change is exacerbating this issue. Stefan highlighted another important point: susceptibility. Air pollution not only drives climate change but also increases host susceptibility to pathogens. Consider COVID-19, which targets the ACE2 receptor in the cardiopulmonary system. Long-term exposure to air pollution can cause cardiopulmonary damage, making individuals more susceptible to such diseases. This scenario is one example of what we might expect in the future. Climate change is pushing human expansion into new areas, which in turn drives further climate change and increases our vulnerability. It’s a perfect storm for future pandemics. In a pessimistic scenario, the outlook is grim unless we take significant action.
Bill Lindsley 1:32:40
I agree with everything that’s been said. Unfortunately, we are likely to encounter some unpleasant surprises in the future.
Kenneth Martinez 1:32:48
Alright, I’ll quickly wrap this up with an observation. I remember from Stefan’s slide deck, he mentioned CO2 concentrations. He noted that the normal CO2 rates in parts of the country are now at 450 parts per million. When I started conducting indoor air quality studies for the National Institute for Occupational Safety and Health (NIOSH) 30 years ago, the average was 250 parts per million. It’s almost doubled in that 30-year period. So, to recap today’s discussion, I want to thank our panelists for their excellent presentations and informative discussions. Thank you all for participating. In closing, I’d like to mention more about our nonprofit, the Integrated Bioscience and Built Environment Consortium. As Coby mentioned, we are focused on buildings, pathogens, and people, aiming to make a difference. We are a membership-based organization, seeking more people to join us. We have four more “lessons learned” sessions in our series, and if anyone is interested in sponsoring these along with the American Industrial Hygiene Association (AIHA), please reach out to us. We are also inviting committee members to join our leadership team and Science Advisory Board. As a member, you can participate in panel sessions like today’s, meet leading professionals in your field, and make your science and knowledge accessible to those who need safer indoor air. Our focus is on pathogens, a crucial subset of indoor air quality, especially relevant now as COVID-19 has heightened awareness of infectious diseases and their impact on our communities, families, and nations. Coby, would you like to add anything in closing? If not, thank you all for your participation. Take care, and I look forward to seeing you in a couple of months when we focus on ventilation.
Watch the other sessions of the 6-part IAQ CLEAN Lessons Learned series
Navigating the H5N1 Challenge
Go to this sessionThe Critical Role of IAQ in Infection Prevention
Go to this sessionBridging the Gap Between Current IAQ Assessments and Evolving Biosensing Technologies in Built Environments
Go to this sessionVentilation as a Key Defense Against Infectious Diseases
Go to this sessionIndoor Air Quality as a Public Health Strategy to Reduce the Risk of Infectious Disease Transmission in the Built Environment
Go to this sessionSponsor Spotlight

American Industrial Hygiene Association (AIHA)
AIHA is the association for scientists and professionals committed to preserving and ensuring occupational and environmental health and safety (OEHS) in the workplace and community. Founded in 1939, we support our members with our expertise, networks, comprehensive education programs, and other products and services that help them maintain the highest professional and competency standards. More than half of AIHA’s nearly 8,500 members are Certified Industrial Hygienists, and many hold other professional designations. AIHA serves as a resource for those employed across the public and private sectors and the communities in which they work.
Have a question about the event?
Connect with IBEC experts directly! Drop your queries below, and let's further the dialogue on preventing the spread of infectious diseases.